# Learning objectives
- To understand the subsets of patients with severe aortic stenosis who do not meet the classical criteria for the diagnosis
了解不符合经典诊断标准的严重主动脉瓣狭窄患者的亚组 - To understand the investigation algorithms for these subsets
了解这些亚组的检查方法 - To discuss the prognosis and surgical/interventional management of these patient sub-groups
讨论这些亚组患者的预后和手术 / 介入治疗
# Difficult Sub-Groups DISCORDANT MEASUREMENTS 测量不一致的困难亚组
# LOW FLOW STATES (LOW LVOT FLOW) 低血流状态 (低 LVOT 流量)
More challenging when AVA does not match gradient
当主瓣面积与压差不匹配时更具挑战性Require further assessment and investigation
需要进一步评估和检查2 distinct clinical entities are seen
可以看到 2 个不同的临床类型- Reduced LVEF 射血分数降低
- Low Flow, Low Gradient Severe AS with impaired LVEF - discussed in Aortic Stenosis lecture
低血流、低压差与左心室射血分数受损的重度 AS - Pseudo-severe AS
假性重度 AS
- Low Flow, Low Gradient Severe AS with impaired LVEF - discussed in Aortic Stenosis lecture
- Normal EF 射血分数正常
- Paradoxical Low Flow Low Gradient Severe AS (normal EF)
矛盾的低流量低压差的严重 AS(正常 EF) - Normal flow Low Gradient Severe AS
正常流量、低压差的严重 AS
- Paradoxical Low Flow Low Gradient Severe AS (normal EF)
- Reduced LVEF 射血分数降低
# HIGH FLOW STATES (HIGH LVOT FLOW) 高血流状态 (高 LVOT 流量)
Valve area may be > 1.0 cm despite a peak velocity > 4 m/s and mean gradient > 40 mmHg in the presence of a HIGH trans-valvular flow
尽管峰值速度大于 4 m/s,平均跨瓣压差大于 40 mmHg,但在高跨瓣流量情况下,瓣膜面积可能大于 1.0 cm- AR? 主动脉瓣反流
- Consider causes of high CO, such as fever and anaemia
考虑高心输出量的原因,如发烧和贫血
Usually, the haemodynamics of gradient and velocities would be consistent with significant AS in these situations
通常,在这些情况下,压差和速度的血流动力学与显著的 AS 一致Need to account for V1 in the Bernoulli equation when V1 > 1.5ms-1
当 V1 > 1.5ms-1 时,需要在伯努利方程中考虑 V1
i.e.V1 = proximal velocity (peak LVOT) 近端血流速度 (LVOT 峰值)
and V2 = distal velocity 远端速度
# Discrepancies in the values obtained 测量值存在差异时
# Measurement taken are incorrect/inaccurate 需要考虑测量结果不正确 / 不准确的情况
- Low echogenicity or severe calcifications
低回声或严重钙化 - AF - beat to beat variation
房颤 - 每次搏动之间的变化 - Sub-aortic stenosis - makes the LVOT velocity incorrect
主动脉瓣下狭窄 - 使 LVOT 速度不正确 - Low or high Cardiac output states
低或高心输出量状态 - Difficult LVOT measurements
LVOT 测量困难
# Critical Issues 关键问题
LVOT diameter incorrect:LVOT 直径不正确
- Underestimation leads to falsely low AVA
低估会导致错误的低主瓣面积 - Discussed in Aortic Stenosis lecture
- Underestimation leads to falsely low AVA
LVOT velocities incorrect: LVOT 速度不正确
- Sub-aortic pathologies 主动脉瓣下病变
- If underestimated can lead to a false diagnosis of low flow low gradient AS
如果低估会导致低流量低压差的错误诊断
Recheck LVOT measurement 重新检查 LVOT 测量
Perform TOE for LVOT measurement 使用经食道超声测量
Consider CT scan or invasive catheterisation as alternative assessment technique.
考虑将 CT 扫描或有创插管作为替代评估技术。
| Low gradient | High Gradient | |
|---|---|---|
Normal flow | "Normal Flow - Low Gradient Severe AS and preserved EF" | Classical Severe Aortic Stenosis |
Low flow | Severe AS with normal EF | Severe Aortic Stenosis with Low flow |
# Stages of
# Progression of VHD 瓣膜性心脏病的发展阶段
| Stage | Definition | Description |
|---|---|---|
A | At risk | Patients with risk factors for the development of VHD |
B | Progressive | Patients with progressive VHD (mild-to-moderate severity and asymptomatic) |
C | Asymptomatic severe 无症状重症 | Asymptomatic patients who have reached the criteria for severe VHD |
| ||
| ||
D | Symptomatic severe 有症状重症 | Patients who have developed symptoms as a result of VHD |
# Valvular Aortic Stenosis 主瓣狭窄的发展阶段
| Stage | Definition | Valve Anatomy | Valve Hemodynamics | Hemodynamic Consequences | Symptoms |
|---|---|---|---|---|---|
A | At risk of AS |
|
|
|
|
B | Progressive AS |
|
|
|
|
| C - Asymptomatic severe AS 无症状重度 AS | |||||
C1 | Asymptomatic severe AS |
|
|
|
|
C2 | Asymptomatic severe AS with LV dysfunction |
|
|
|
|
| D - Symptomatic severe AS 症状性重度 AS | |||||
D1 | Symptomatic severe high-gradient AS |
|
|
|
|
D2 | Symptomatic severe low-flow/low-gradient AS with reduced LVEF |
|
|
|
|
D3 | Symptomatic severe low-gradient AS with normal LVEF or paradoxical low-flow severe AS |
|
|
|
|
Classification and Characterisation of the Different Types of AS According to AVA, Gradient, LVEF, and Flow [1]
根据 AVA、压差、LVEF 和血流对不同类型 AS 的分类和特征
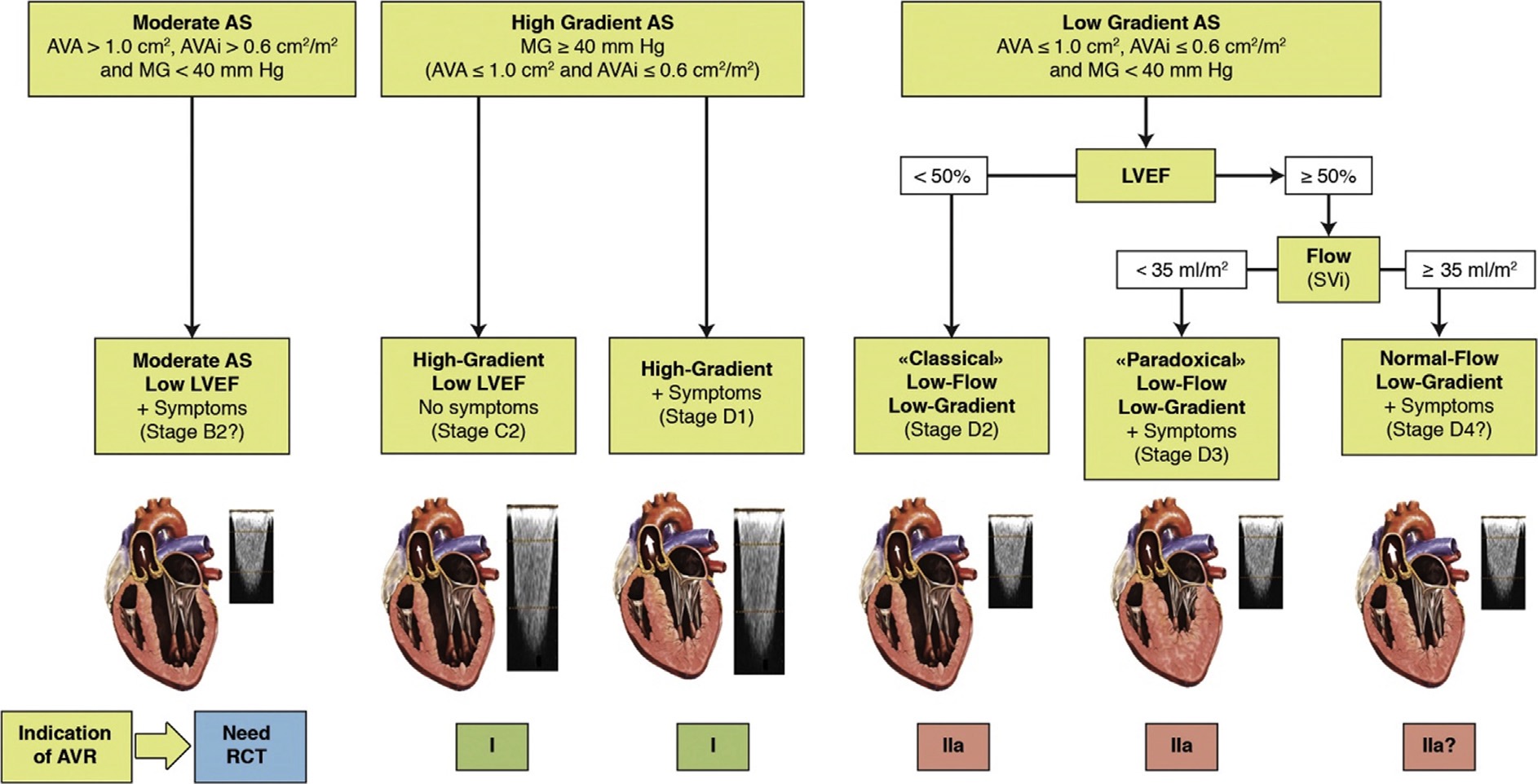
- Classification of types of AS, including only the categories associated with symptoms and/or depressed LVEF.
AS 类型的分类,仅包括与症状和 / 或左心室射血分数降低相关的类别。 - It does not include stage C1 (i.e., patients with high-gradient AS, no symptoms, and preserved LVEF).
不包括 C1 期 (即高阶梯度型 AS 患者,无症状,左心室射血分数保留) - Question mark indicates stage labels or indications for aortic valve replacement (AVR) that are proposed but are not included in the guidelines and will need to be further tested and validated.
问号表示主动脉瓣置换术(AVR)的阶段标签或适应症,建议但未包含在指南中,需要进一步测试和验证。 - AVAi, Indexed AVA 主动脉瓣面积指数;MG, mean gradient; RCT, randomized controlled trial; SVi, stroke volume index.
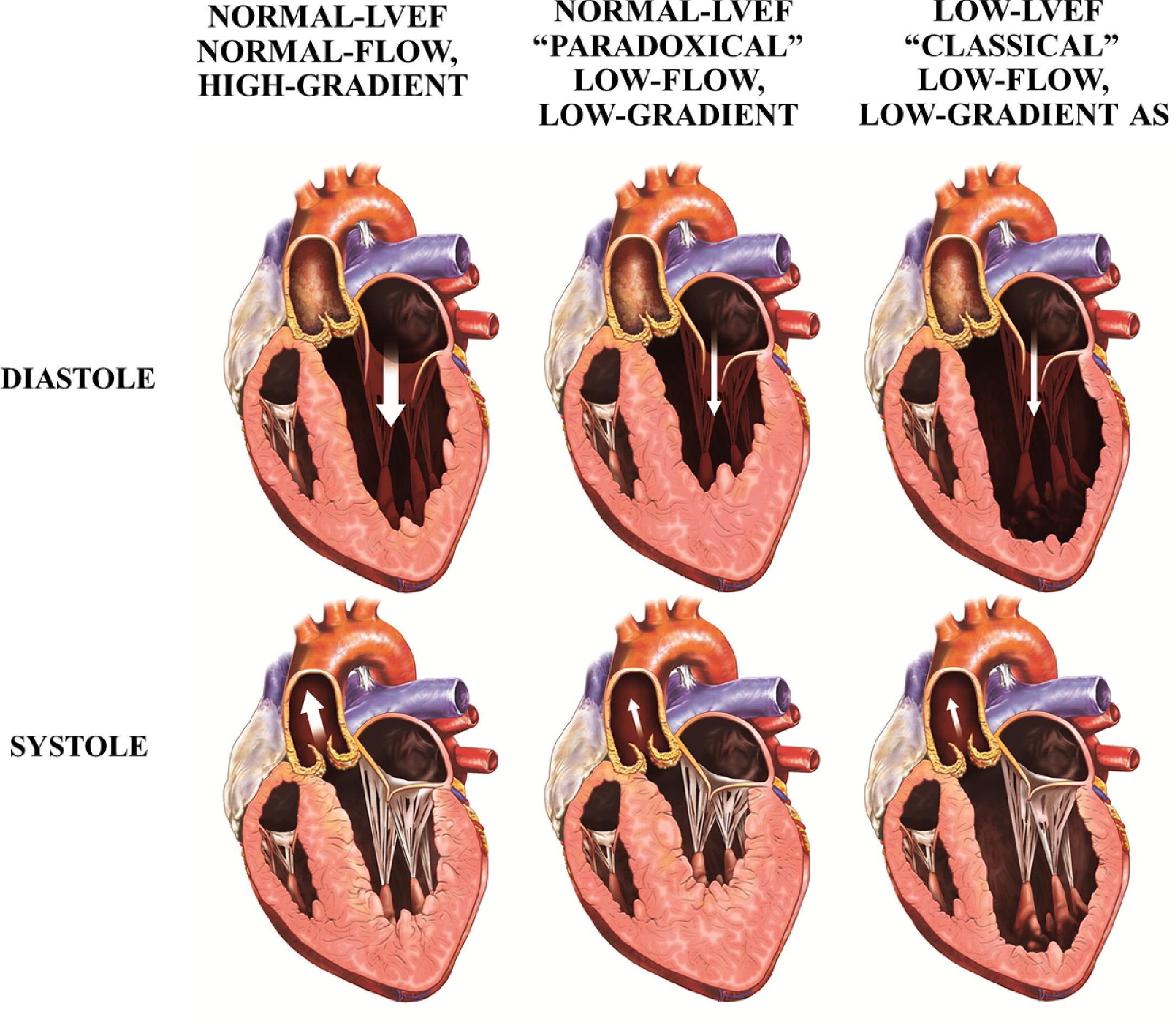
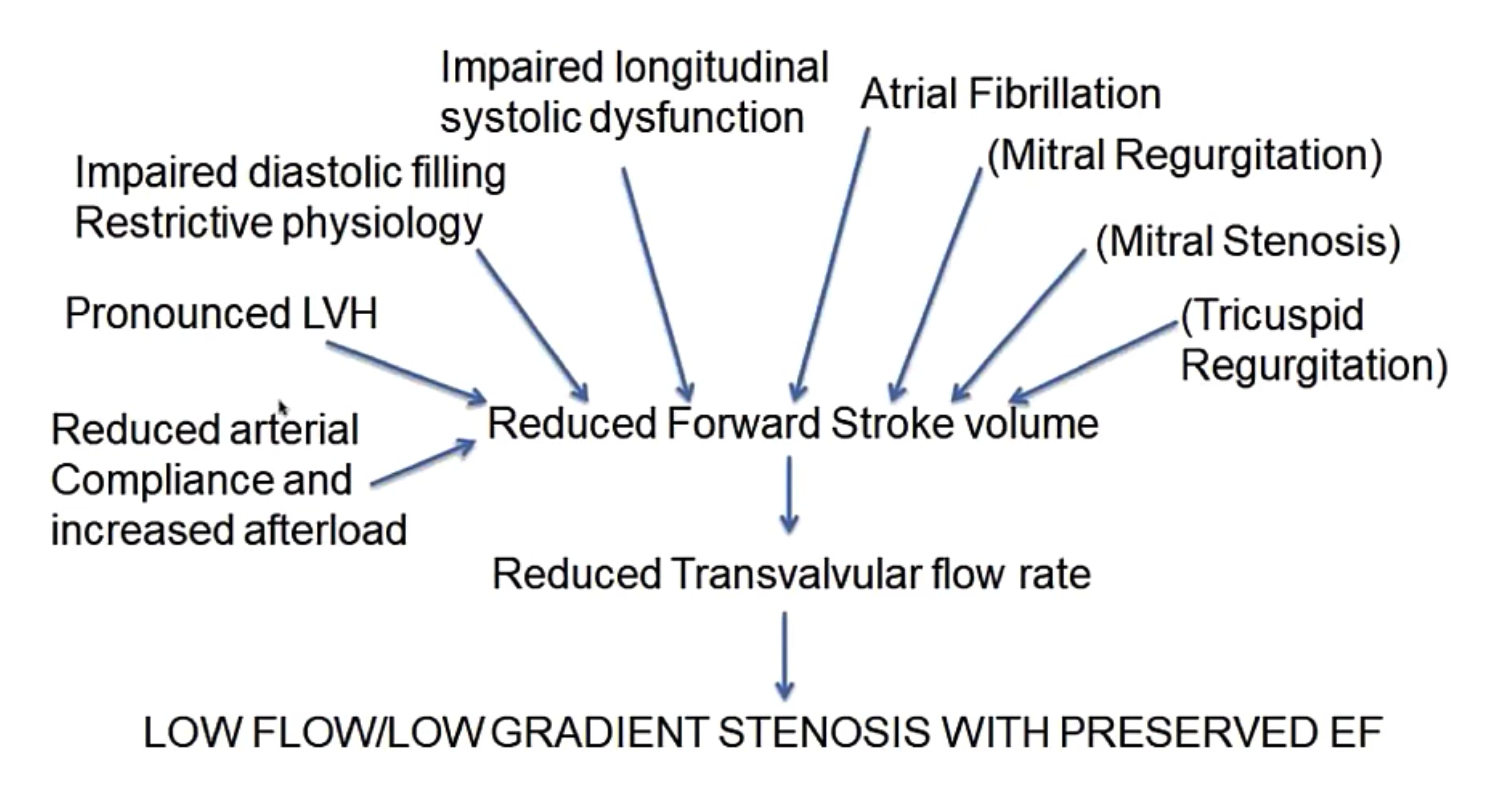
# Paradoxical Low Flow-Low Gradient Severe Aortic Stenosis 矛盾性 LFLG AS
Some patients with severe aortic stenosis based on valve area have a lower-than-expected gradient (e.g. mean gradient < 30 mmHg) despite preserved ejection fraction (e.g. EF > 50%)
尽管射血分数维持正常(如 EF>50%),一些严重主动脉瓣狭窄的患者的跨瓣压差低于预期(如平均压差 < 30 mmHg)Up to 35% of patients with severe aortic stenosis present with low flow, low gradient; 5% to 15% of AS patient have paradoxical LF/LG
高达 35% 的重度主动脉狭窄患者表现为低流量、低压差;5% 至 15% 的 AS 患者存在矛盾性的 LF/LGThese low gradients often lead to an underestimation ol the severity of the disease, so many of these patients do not undergo surgical aortic valve replacement.
这些低压差常常导致对疾病严重程度的低估,因此这些患者中的许多人没有接受主动脉瓣置换手术。How is this possible? 为何会如此
- High global afterload - Especially elderly with reduced systemic arterial compliance. HYPERTENSION
整体后负荷高 - 尤其是全身动脉顺应性降低的老年人。高血压 - LV longitudinal dysfunction despite normal LVEF
尽管 LVEF 正常,但左室纵向功能障碍 - Diastolic dlysfunction - especially restrictive physiology
左室舒张功能 - 特别是限制性生理学 - Reduced LV cavity size due to severe LVH
由于严重的左心室肥厚,减少了左心室腔大小 - Higher LV mass than NF/HG (concentric hypertrophy)
左心室质量高于 正常血流 / 高跨瓣压差 (向心性肥厚) - Reduced cardiac output and normalisation of peripheral blood pressure
心输出量减少和外周血压正常化 - More AF
房颤
- High global afterload - Especially elderly with reduced systemic arterial compliance. HYPERTENSION
In general, this is a more advanced stage of the disease process
总的来说,这是疾病过程的更高级阶段- Older; women; hypertension history; Diabetes or metabolic syndrome.
老年;女性;高血压史;糖尿病或代谢综合征。
- Older; women; hypertension history; Diabetes or metabolic syndrome.
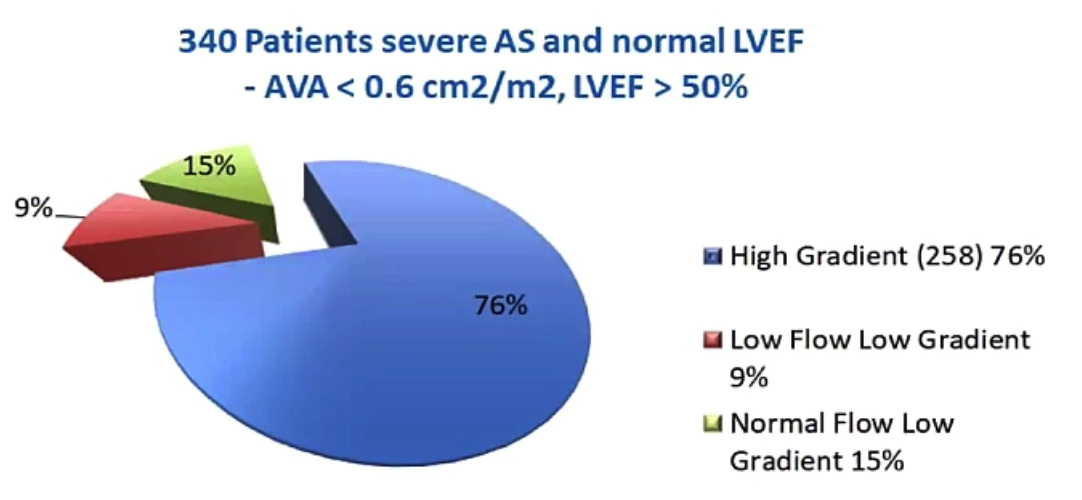
AS in patients with normal LVEF Low Flow Low Gradient AS relatively uncommon [2] (高压差 76%,低血流低压差占 9%,正常血流低压差占 15%)
# Echo Doppler Features of Paradoxical Low-Flow, Low-Gradient AS 超声表现
The Aortic Valve: 主瓣本身 [3]
- AVA, aortic valve area 主动脉瓣面积 < 1.0 cm2
- AVAi, aortic valve area index 主动脉瓣面积指数 < 0.6 cm2/m2
- DVI, Doppler Velocity Index 多普勒速度指数 < 0.25
- Severely thickened/calcified valve 严重增厚 / 钙化瓣膜
- MG, mean gradient 平均跨瓣压差 < 40 mmHg
- ZVA, Valvulo-arterial impedance 瓣膜动脉阻抗 ≥ 4.5
The Left Ventricle: 左室腔
- EDD 舒张末内径 < 47 mm
- EDV 舒张末容积 < 55 mL/m2
- RWT ratio 相对室壁厚度 > 0.50
- Myocardial fibrosis 心肌纤维化
- Impaired LV filling 左室充盈受损
- LVEF > 50%
- GLS 整体应变率 ≤ 15%
- SVi, stroke volume index 每搏量指数 < 35mL/m2
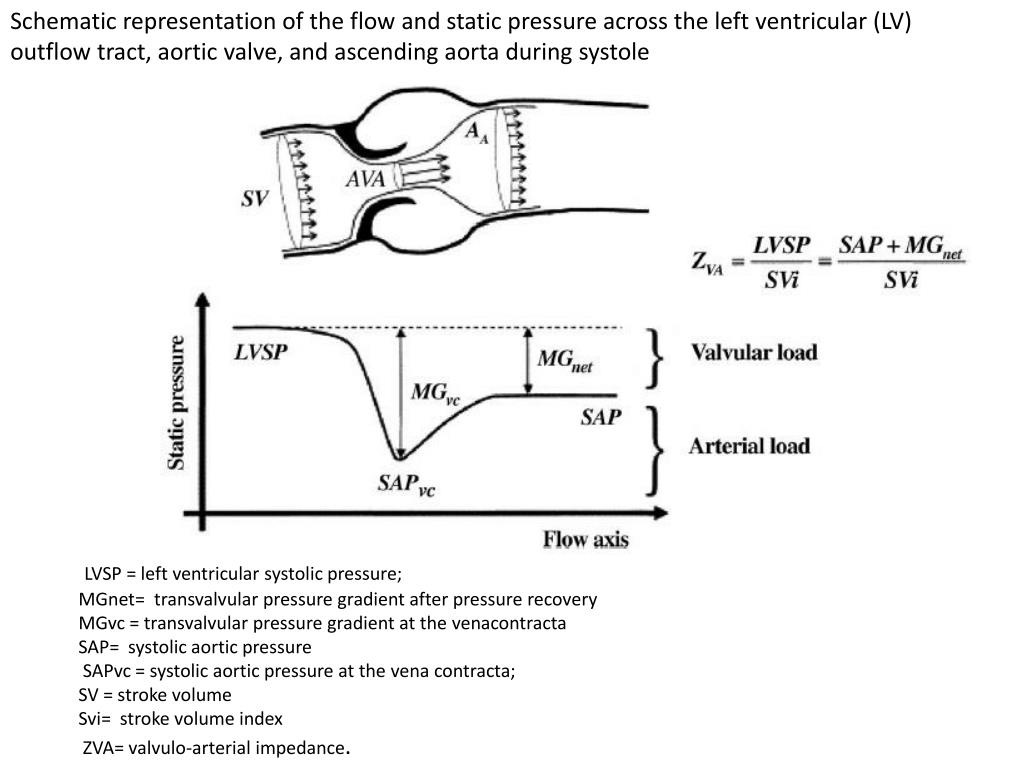
# What is Valvulo-Arterial Impedance ZVA 瓣膜 - 动脉阻抗?
ZVA provides an estimate of the global haemodynamic load that results from the summation of the valvular and vascular loads.
ZVA 提供了由瓣膜和血管负荷之和产生的整体血流动力学负荷的估计值Influenced by: 受到以下影响
- Stenosis severity 狭窄的严重程度
- Volume flow rate 容积血流率
- Body size 身体大小
- Systemic vascular resistance 全身血管阻力
Measuring ZVA in Aortic Stenosis
![]()
- LVSP, left ventricular systolic pressure 左室收缩压
- SVi, stroke volume index 每搏量指数
- SAP, systolic aortic pressure 主动脉收缩压
- MG, mean gradient 平均跨瓣压差
- Systemic arterial compliance calculated as the ratio of stroke volume index to arterial pulse pressure
以每搏输出量指数与动脉脉压之比计算全身动脉顺应性
| > 3.5 | Moderate |
| ≥ 4.5 | Severe |
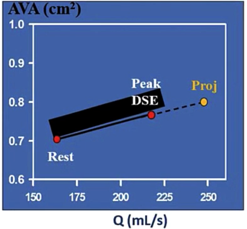
# Ensure this is not just moderate AS 确保这不仅仅是中度 AS
- i.e. not pseudo-severe LF/LG AS
比如不是假性重症 LF/LG AS - 33% of these patients may be pseudo severe
33% 的患者可能为假性重症 - Like low gradient low EF patients useful ways to investigate are:
像低压差低 EF 患者一样,有用的检查方法有:- Dobutamine infusion - LESS VALIDATED - only 1 study
多巴酚丁胺注射 - 验证较少 - CT calcium scoring CT 钙化评分
- Dobutamine infusion - LESS VALIDATED - only 1 study
- Additional studies still needed in this evolving field.
在这个不断发展的领域中,仍然需要进行更多的研究。
# Stress Echocardiography
- to Differentiate True vs. Pseudo-Severe Stenosis in Paradoxical, Low-Flow, Low-Gradient AS [4]
多巴酚丁胺负荷超声
# Normal Flow-Low Gradient Group 正常血流低压差组
- Heterogeneous but commonest of low gradient group
异质但最常见的低压差组 - Severe AS less likely
严重的可能性较小 - More commonly female:
女性更常见的:- Small body size patients; small LVOT area
体型较小的患者;左心室流出道面积较小 - Fluid dynamic inconsistencies in the gradient-area guideline
梯度面积指南中的流体动力学不一致- 40mmHg mean gradient cut-off may be too high??
40mmHg 平均压差作为分界可能太高??
- 40mmHg mean gradient cut-off may be too high??
- AF/ prolonged LV ejection time
房颤 / 左室射血时间延长
- Small body size patients; small LVOT area
- Many (50%) will have moderate AS
许多 (50%) 有中度 AS - Less severe AS/ less advanced disease state
不太严重的 AS / 不太严重的疾病状态 - Consider further tests if AVA < 0.6 cm2
如果 AVA < 0.6 cm2,请考虑进一步检查- i.e., with more stringent criteria for severe AS.
对严重 AS 有更严格的标准。 - LVEF ≥ 50%, a normal flow state (stroke volume index 235 ml/m2), an AVA ≤1.0 cm2, an indexed AVA ≤ 0.6 cm2/m2, and a mean gradient < 40 mmHg
- i.e., with more stringent criteria for severe AS.
- if AVA < 0.6 cm2 then consider
- DSE 多巴酚丁胺负荷超声心动图
- CT calcium scoring CT 钙化评分
- Patients with true severe AS NF/LG group benefit from surgery.
真正重度 AS 组的患者可从手术中获益
# LF/HG Group 低血流高压差组
- LF is affected by high body surface area and excess weight
LF 受到高体表面积和超重的影响 - obesity (c. 80% obese) 肥胖 80% 存在 [5]
- i.e. absolute stroke volume(SV) is normal, but high BSA leads to low stroke volume index(SVi)
绝对每搏量是正常的,但高 BSA 会导致低每搏量指数
- i.e. absolute stroke volume(SV) is normal, but high BSA leads to low stroke volume index(SVi)
- Higher mortality compared to NF/HG perhaps related to these comorbidities:
与 NF/HG 相比,死亡率更高可能与这些合并症有关:- Obesity 肥胖
- DM 糖尿病
- AF 房颤
- Heart failure presentations 心力衰竭表现
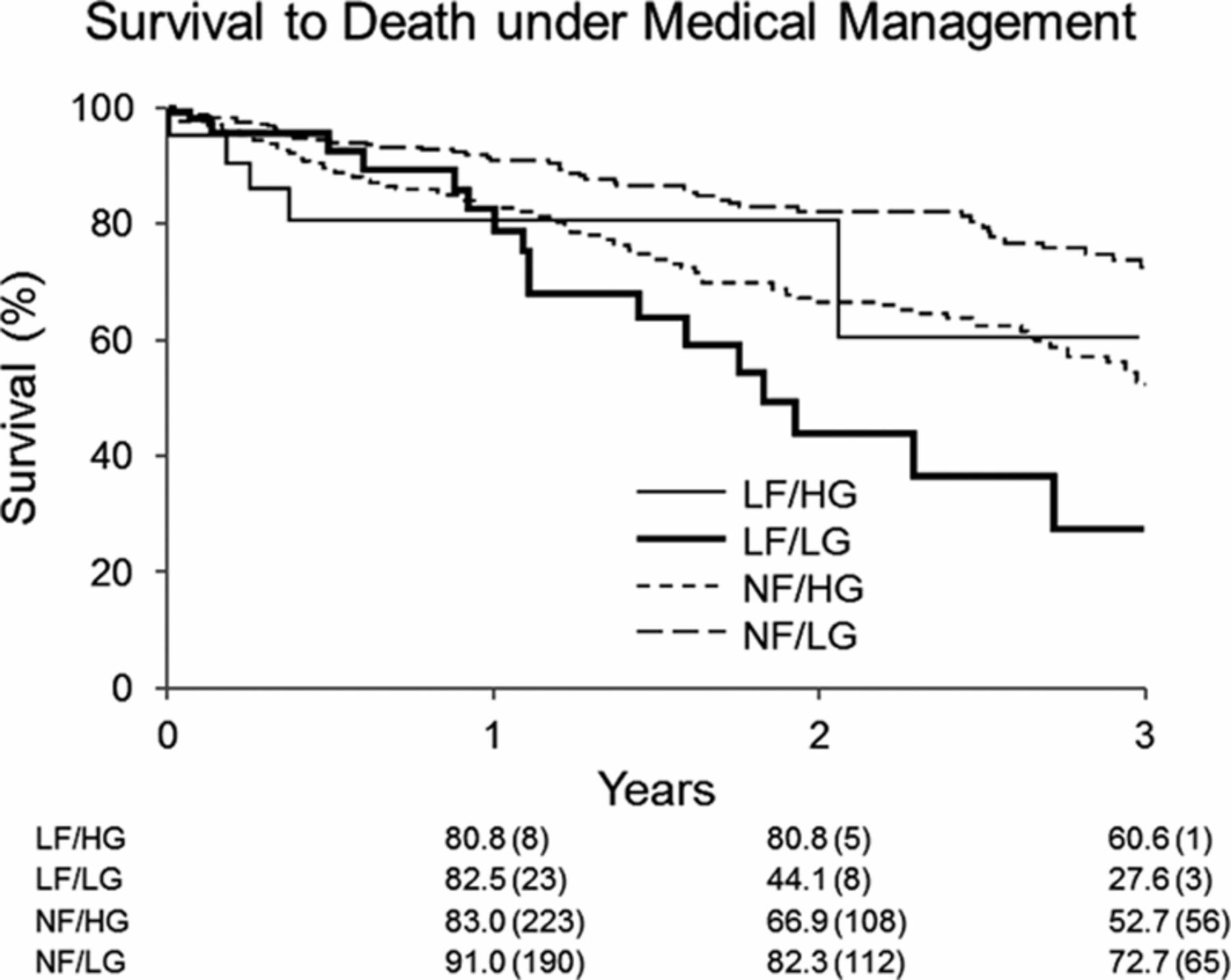
# Prognosis-medical management 预后 - 医疗管理
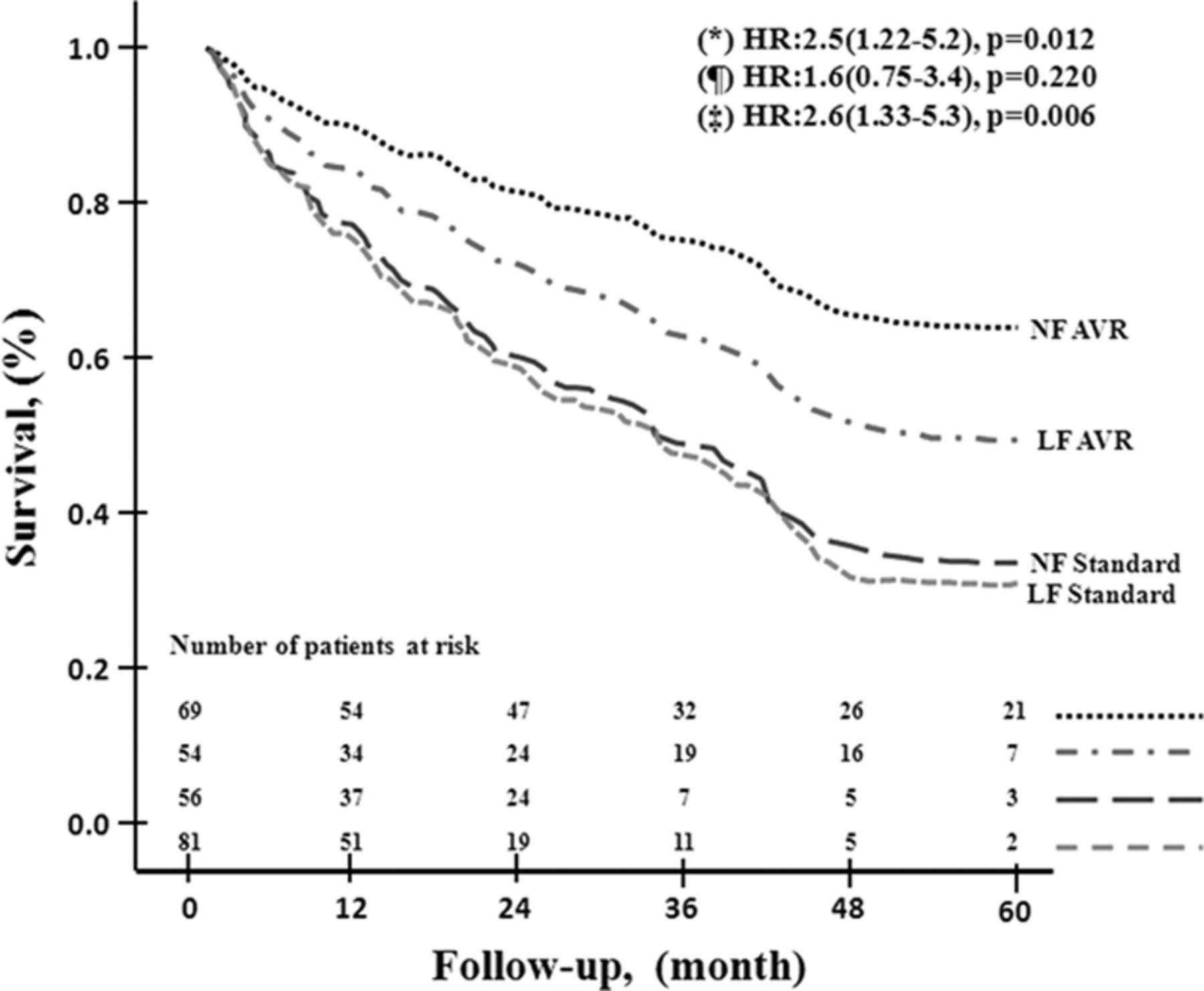
AVR was beneficial in both LF and NF groups [6]
不管是低血流还是正常血流,主动脉瓣置换都可以使重度 AS 受益Low flow states are an independent predictor of poor outcome [5]
低流量状态是不良结局的独立预测因素Independent of gradient or LVEF
与压差或 LVEF 无关LF/LG worst outcome 3.2x increase mortality compared to NF/LG
与 NF/LG 相比,LF/LG 最差结局死亡率增加 3.2 倍
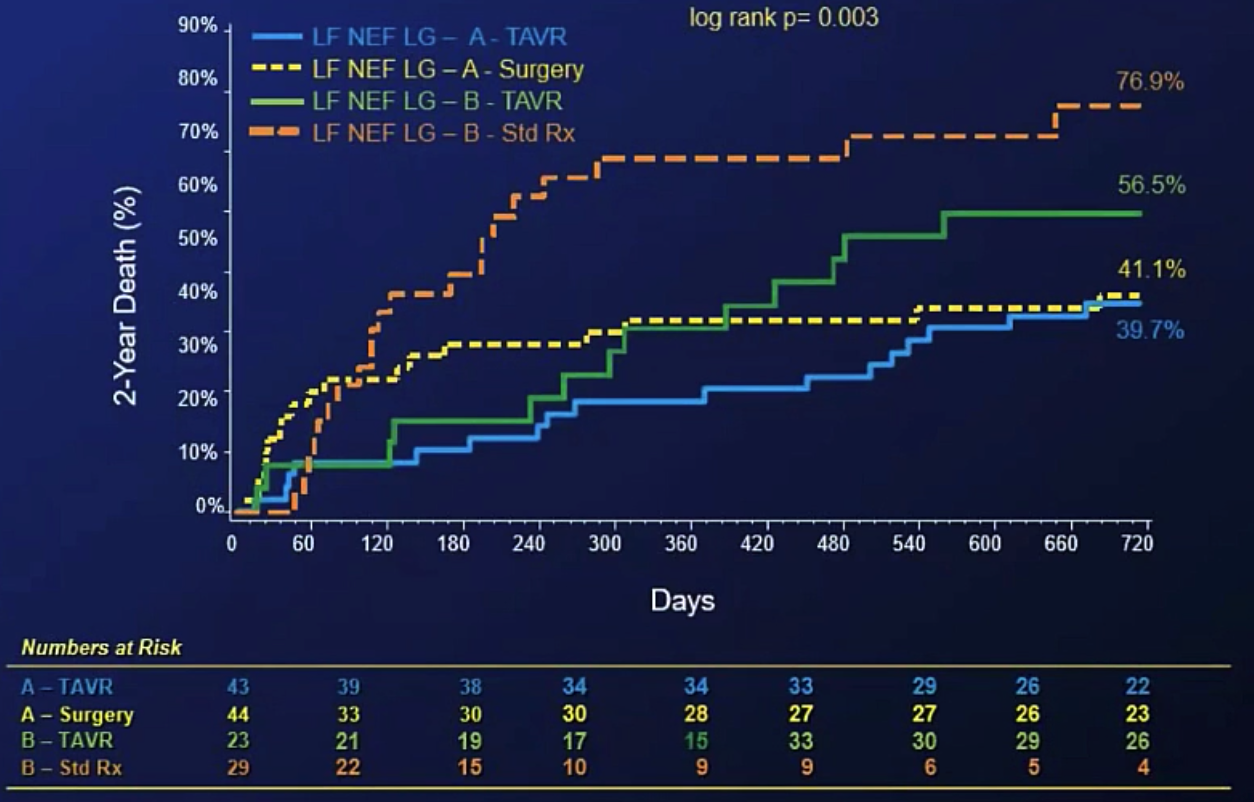
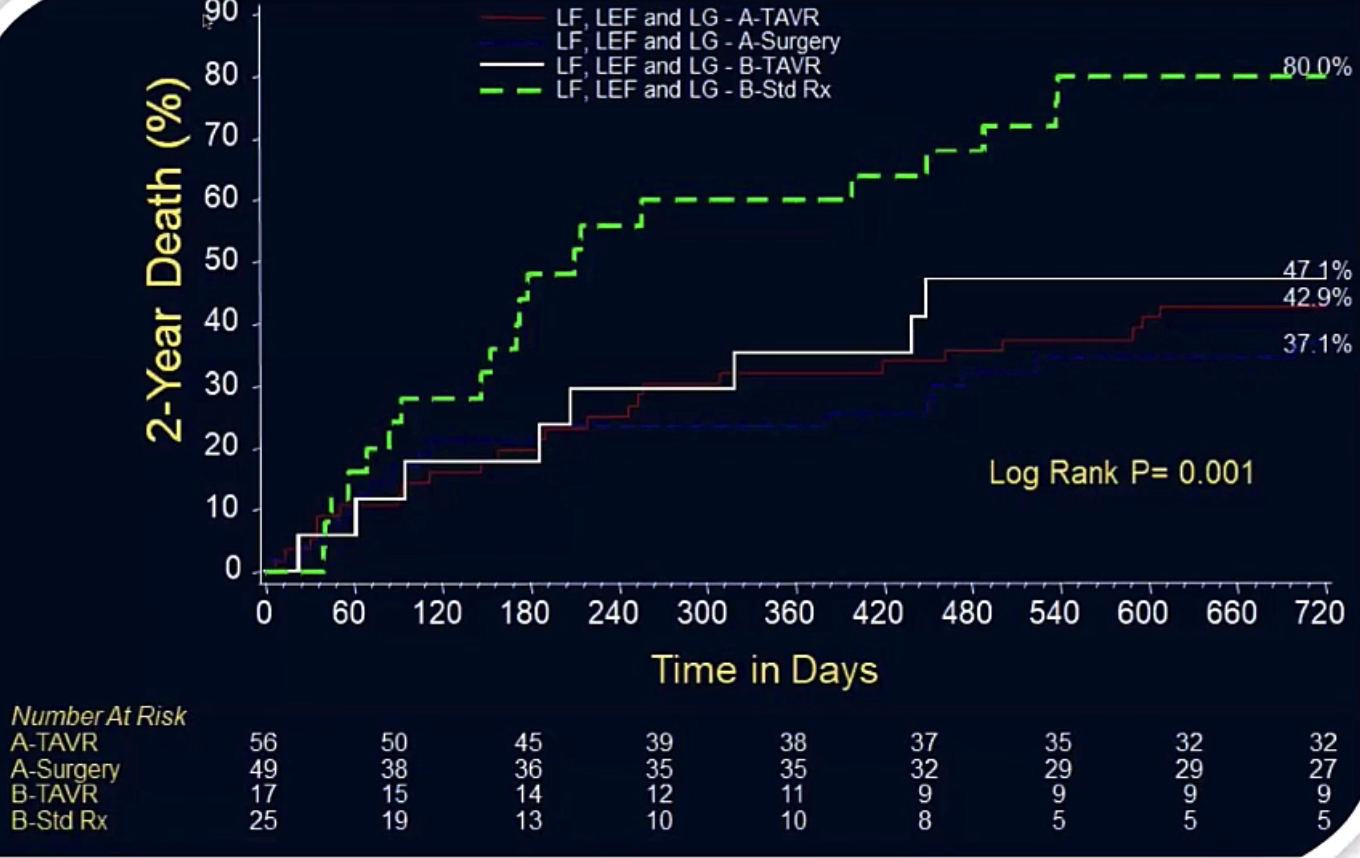
- Partner 1 cohort B (non-operable): TAVI resulted in large benefit for these LF/LG patient survival
TAVI 为这些 LF/LG 患者的生存带来了巨大的好处 - TAVI Treatment Comparison in LF, LEF, and LG (both cohorts)
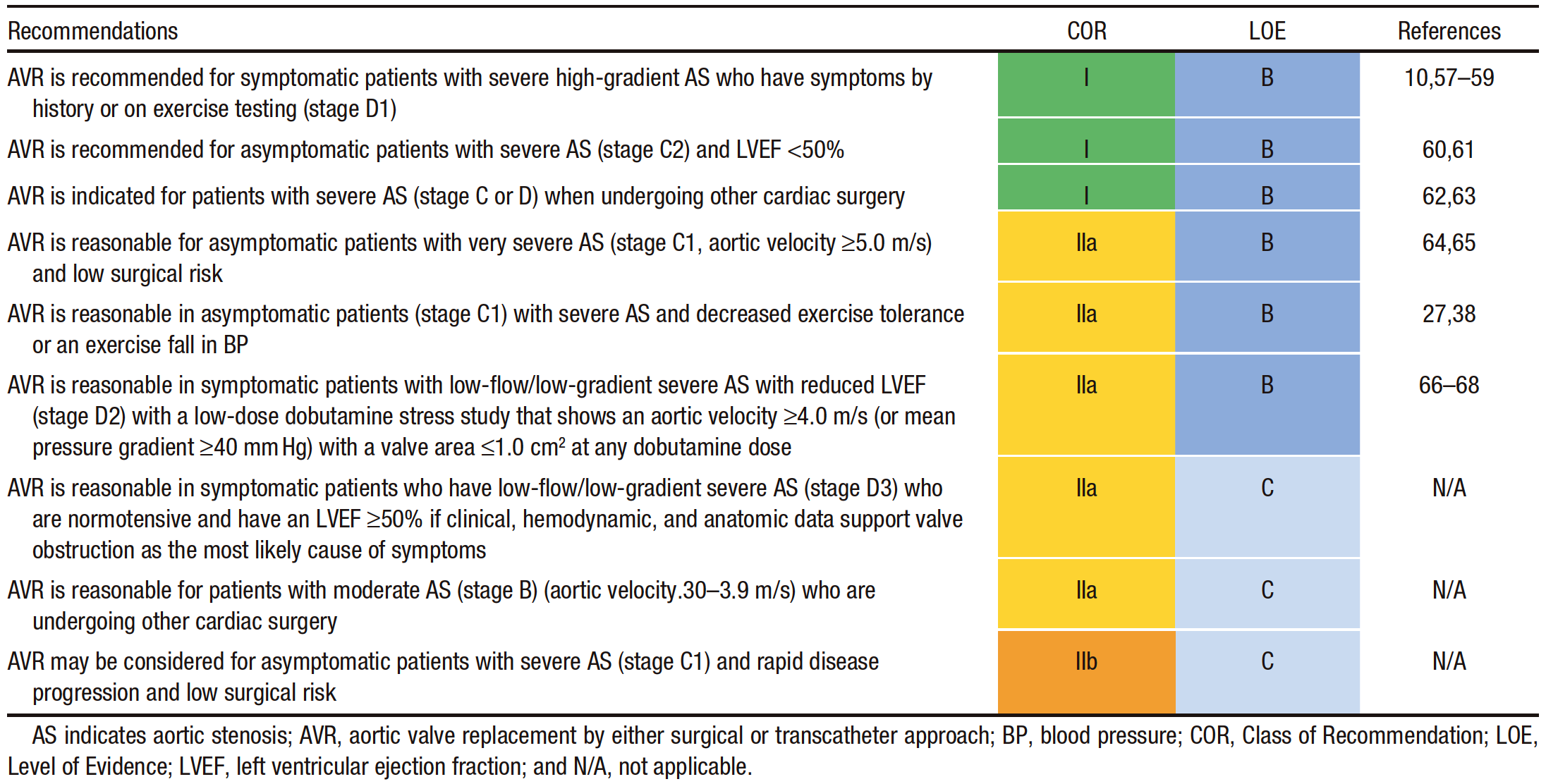
Summary ot Recommendations for AS: Timing of Intervention [7] 干预时机
![]()
AVR is reasonable in symptomatic patients who have low-flow/low-gradient severe AS (stage D3) who are normotensive and have an LVEF ≥50% if clinical, hemodynamic, and anatomic data support valve obstruction as the most likely cause of symptoms
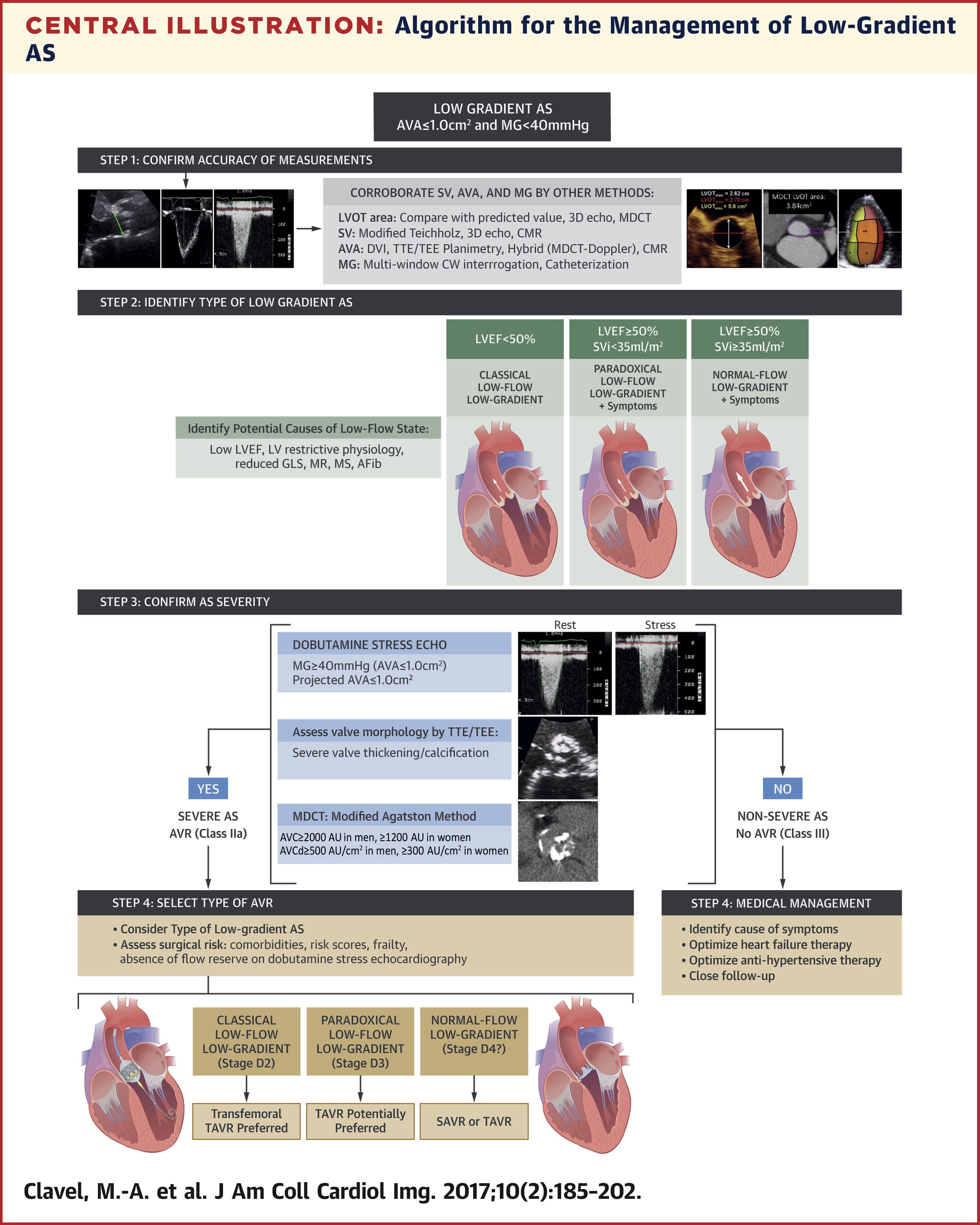
如果临床、血液动力学和解剖学数据支持瓣膜阻塞是最常见的症状原因,AVR 对低流量 / 低压差严重 AS(D3 阶段)有正常血压且 LVEF≥50% 的有症状患者来说是合理的Algorithm for the Management of Low-Gradient AS [4]
![]()
Hahn, R. T., Nicoara, A., Kapadia, S., Svensson, L., & Martin, R. (2018). Echocardiographic Imaging for Transcatheter Aortic Valve Replacement. Journal of the American Society of Echocardiography, 31(4), 405–433. ↩︎
Adda, J., Mielot, C., Giorgi, R., Cransac, F., Zirphile, X., Donal, E., Sportouch-Dukhan, C., Réant, P., Laffitte, S., Cade, S., Le Dolley, Y., Thuny, F., Touboul, N., Lavoute, C., Avierinos, J. F., Lancellotti, P., & Habib, G. (2012). Low-flow, low-gradient severe aortic stenosis despite normal ejection fraction is associated with severe left ventricular dysfunction as assessed by speckle-tracking echocardiography: a multicenter study. Circulation. Cardiovascular imaging, 5(1), 27–35. ↩︎
Pibarot, P., & Dumesnil, J. G. (2011). Paradoxical low-flow, low-gradient aortic stenosis adding new pieces to the puzzle. Journal of the American College of Cardiology, 58(4), 413–415. ↩︎
Clavel, M. A., Ennezat, P. V., Maréchaux, S., Dumesnil, J. G., Capoulade, R., Hachicha, Z., Mathieu, P., Bellouin, A., Bergeron, S., Meimoun, P., Arsenault, M., Le Tourneau, T., Pasquet, A., Couture, C., & Pibarot, P. (2013). Stress echocardiography to assess stenosis severity and predict outcome in patients with paradoxical low-flow, low-gradient aortic stenosis and preserved LVEF. JACC. Cardiovascular imaging, 6(2), 175–183. ↩︎ ↩︎
Eleid, M. F., Sorajja, P., Michelena, H. I., Malouf, J. F., Scott, C. G., & Pellikka, P. A. (2013). Flow-gradient patterns in severe aortic stenosis with preserved ejection fraction: clinical characteristics and predictors of survival. Circulation, 128(16), 1781–1789. ↩︎ ↩︎
Ozkan, A., Hachamovitch, R., Kapadia, S. R., Tuzcu, E. M., & Marwick, T. H. (2013). Impact of aortic valve replacement on outcome of symptomatic patients with severe aortic stenosis with low gradient and preserved left ventricular ejection fraction. Circulation, 128(6), 622–631. ↩︎
Nishimura, R. A., Otto, C. M., Bonow, R. O., Carabello, B. A., Erwin, J. P., 3rd, Guyton, R. A., O'Gara, P. T., Ruiz, C. E., Skubas, N. J., Sorajja, P., Sundt, T. M., 3rd, Thomas, J. D., & ACC/AHA Task Force Members (2014). 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation, 129(23), 2440–2492. ↩︎