# Learning objectives
- Causes of MS
- Cardiac changes in MS
- Assessing MS severity
- Wilkins score/commissural calcification score.
# Role of Echocardiography
- Confirmation of diagnosis and aetiology of MS
MS 的诊断和病因确认 - Quantification of MS severity
MS 严重程度的量化 - Assessment of MS complications
MS 并发症的评估 - Analysis of valve anatomy to determine suitability for percutaneous mitral balloon valvuloplasty/surgery.
分析瓣膜解剖,以确定是否适合经皮二尖瓣膜成形术 / 外科手术
# Cardiac Changes in MS
Right Heart Failure | Pulmonary HTN 肺动脉高压 |
RV Pressure Overload 右室压力负荷过大 | LV Filling ↓ 左室充盈下降 |
# Causes of Mitral Stenosis
- Rheumatic heart disease is the most common cause (85%)
风湿性心脏病是最常见的原因 (85%) - Mitral Annular calcification in 12.5%
二尖瓣环钙化 - Carcinoid heart disease - Predominantly regurgitation
类癌性心脏病 - 主要为反流 - Post MV repair
二尖瓣修复后 - Congenital (0.6%)
先天性 - Rarer: Fabry's, mucopolysaccharidosis, methysergide therapy.
少见:法布里氏病,粘多糖症,甲基色胺治疗
# Rheumatic Mitral Stenosis 风湿性二尖瓣狭窄
Thickening of leaflet edges is the first change in rheumatic MS
瓣叶边缘增厚是风湿性 MS 的第一个变化Fusion of commissures is pathognomonic
病理改变是交界融合Chordae shortening and fusion
腱索缩短和融合Systolic apical displacement of the leaflet closure line in relation to the mitral annular plane
瓣叶闭合线相对于二尖瓣环平面的收缩期尖端位移Calcific deposits
晚期发生钙化沉积物Diastolic doming of the anterior MV leaflet
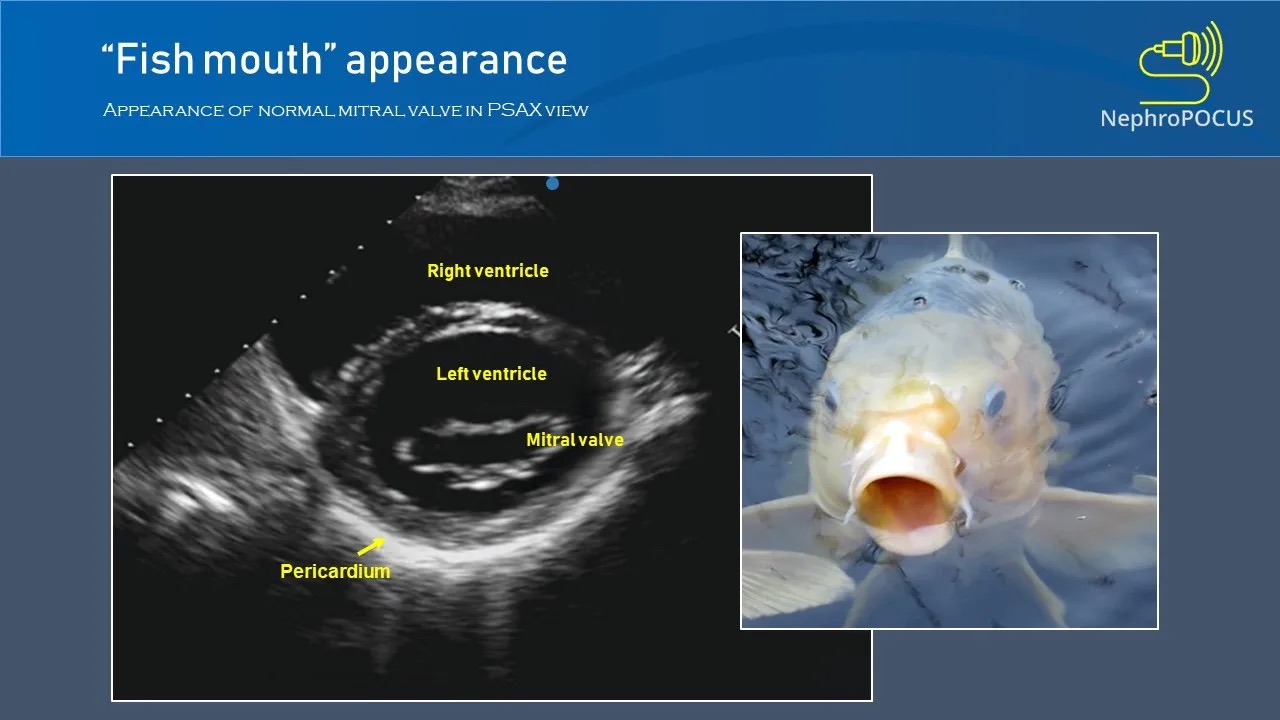
舒张期 LAX,二尖瓣瓣前叶的穹隆样改变Fish mouth appearance of the MV in diastole
舒张期 SAX,MV 的鱼嘴样形态Hockey stick appearance of the anterior MV leaflet
二尖瓣前叶的曲棍球棒外观(类似穹隆样改变)Funnel shape due to complete loss of mobility in the late stages of rheumatic MS.
晚期由于瓣叶完全丧失活动能力,而形成漏斗状。
# Mitral Annulus Calcification 二尖瓣环钙化
因为 MAC 导致狭窄甚至换瓣的病例并不多
- Chronic degenerative process in the fibrous base of the mitral valve (commonly in posterior MV annulus)
慢性退行性变(的钙化)通常位于二尖瓣瓣叶根部的纤维组织 (常见于二尖瓣后瓣环) - MAC is echodense with irregular/lumpy appearance
MAC 表现为回声密集增强,外观不规则 / 团块状 - Associated with acoustic shadow.
重度钙化的下方可能伴有声影的出现
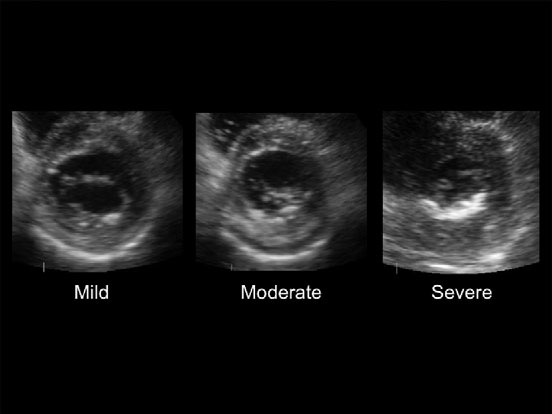
| Grading MAC[1] | 厚度 | 密度 |
|---|---|---|
Mild | < 4mm thickness | limited echodensity of MV annulus |
Moderate | < 4mm thickness | echodensity of≤ of annular ring circumference |
Severe | > 4mm thickness | > annular ring circumference |
- May be accompanied by increase in MPG when restricted anterior MV leaflet.
当前叶受限时,可能伴有平均跨瓣压差升高。
# Congenital Mitral Stenosis 先天性二尖瓣狭窄
- Rare (0.6%) 很少见
- Combined with other congenital defects
常合并其他先天性缺陷 - Parachute mitral valve - Mitral chordae insert into one papillary muscle [2][3]
降落伞样二尖瓣 - 二尖瓣腱索仅附着在一个乳头肌上,瓣叶增厚呈现强回声改变
- Double orifice - Two valve orifices with two separate subvalvular apparatus [4]
双孔二尖瓣 - 带有两套独立的瓣下装置
Annulus hypoplasia 瓣环发育不全
- Hypoplastic left heart with mitral annulus hypoplasia resulting in severe mitral stenosis.
左心发育不全伴二尖瓣环发育不良,导致严重二尖瓣狭窄。
![多见于儿童,成人很少见]()
- Hypoplastic left heart with mitral annulus hypoplasia resulting in severe mitral stenosis.
Associated with complete mitral valve hypoplasia.
与完全性二尖瓣发育不全有关。
# Assessing MS severity 严重程度评估
- M mode
- MVA Planimetry MVA 平面测量法
- Mean pressure gradient 平均压差
- Pressure Half-Time 压力减半时间
仅瓣膜本身,其他伴发改变不再提
# M mode
- Visual assessment of the degree of excursion and leaflet mobility
目测评估偏移程度和瓣叶活动度 - Best assessed in parasternal long axis (leaflets perpendicular)
最好在胸骨旁长轴切面(垂直于瓣叶)评估 - Decreased E-F slope/decreased D-E excursion
E-F 斜率减小 / D-E 漂移减小 - Poor leaflet separation.
前后瓣叶分离不良
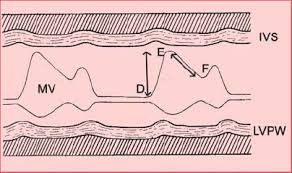
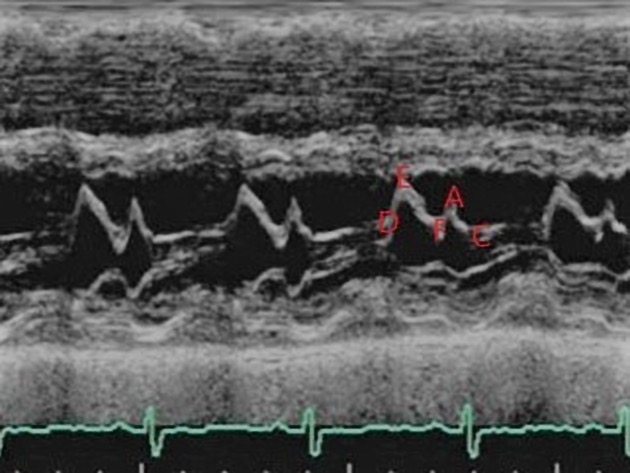
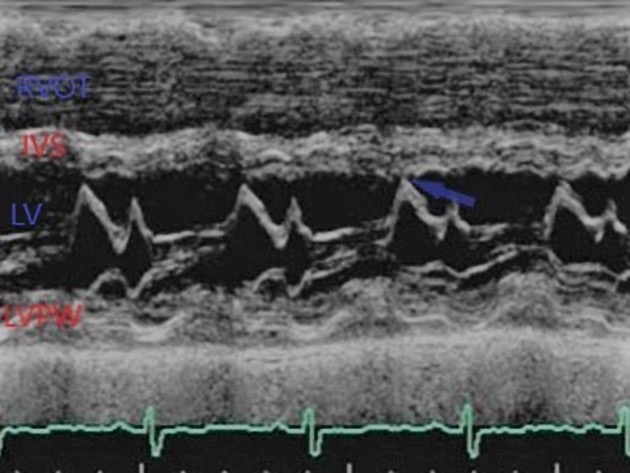
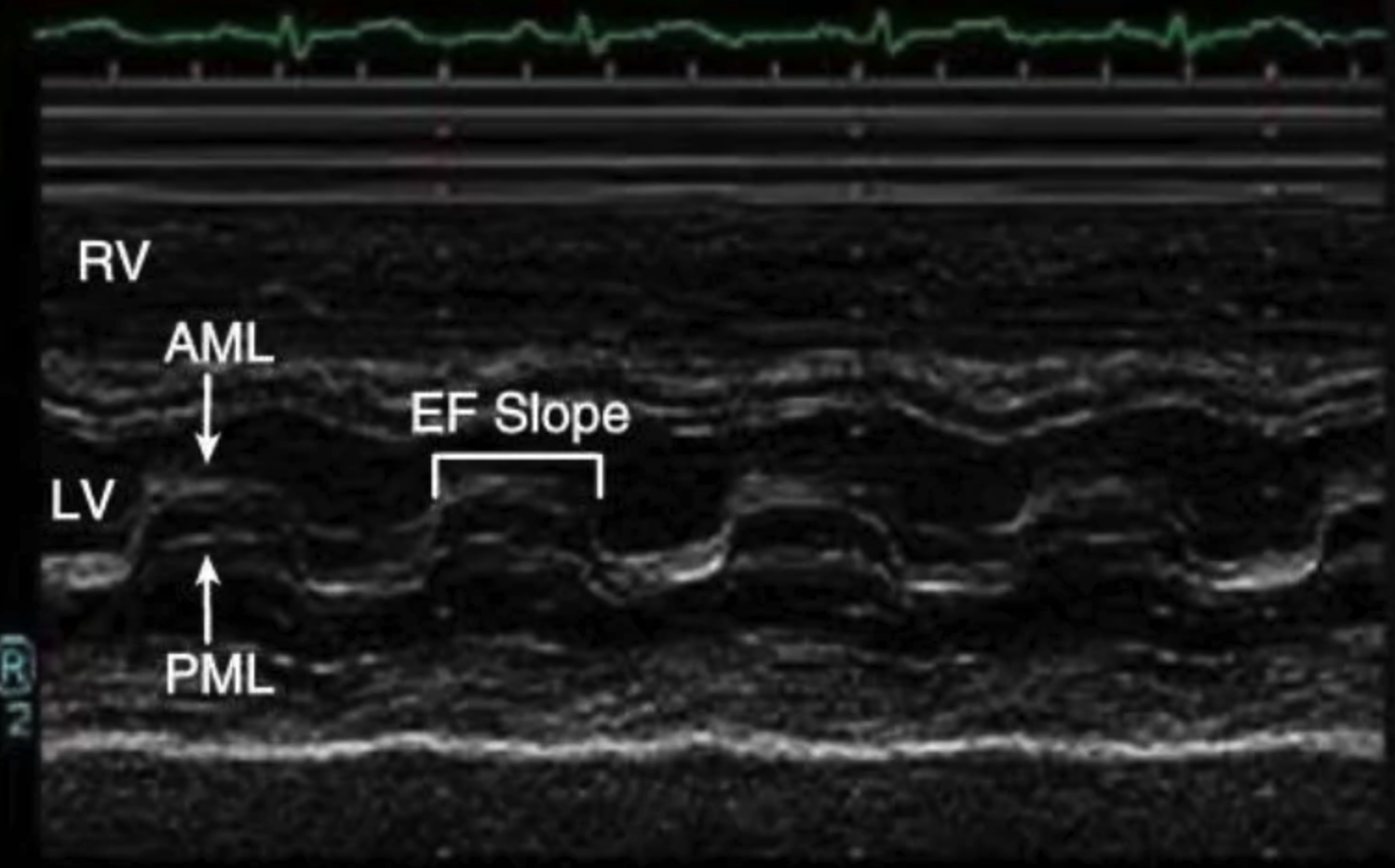
An M-mode echocardiogram from the parasternal long axis, with the m-mode pick directed through the mitral valve leaflets.
胸骨旁长轴的 M 型超声心动图,M 型采样线放在二尖瓣叶尖。One may appreciate the approximated mitral valve leaflets at the beginning of diastole (D) swing apart, with the cephalad and anterior excursion of the anterior leaflet contacting the septum at its peak excursion (E).
在舒张初期(D),我们可以看到二尖瓣瓣叶近似分开,前瓣叶的头部和前部偏移在峰值偏移(E)处接触到中隔。As the pressure gradient between the left atrium and left ventricle begins to decline towards diastasis, the valves return toward their nuclear position (F).
随着左心房和左心室之间的压力梯度开始向舒张下降,瓣膜返回其核心位置 (F)。Their path is then reversed by atrial contraction (A), and thereafter trend toward one another until ventricular systole forces rapid coaptation.
然后它们的路径被心房收缩逆转 (A),然后彼此趋向,直到心室收缩迫使快速接合。Anatomy is labelled as RVOT (right ventricular outflow tract), IVS (interventricular septum), LV (left ventricle), and LVPW (left ventricular posterior wall).
解剖学标记为 RVOT(右心室流出道)、IVS(室间隔)、LV(左心室)和 LVPW(左心室后壁)。Historically, the E-F and A-C slopes were sought as barometers of left ventricular function.
EF 和 AC 斜率被寻求作为左心室功能的晴雨表。Mitral stenosis would classically decrease the E-F slope in the context of an enlarged left atrium, while the latter would be interrupted by a positive deflection ("B bump") in the presence of elevated left ventricular filling pressures.
在左心房扩大的情况下,二尖瓣狭窄通常会降低 EF 斜率,而在左心室充盈压力升高的情况下,后者会被正偏转(“B 凸点”)打断。While the aforementioned parameters are no longer used routinely, E point septal separation (EPSS), the distance between the anterior MV leaflet at its most anterior opening excursion (the E point) and the interventricular septum is a reproducible, quick, and highly sensitive measure of severe left ventricular systolic dysfunction.
虽然上述参数不再常规使用,但 E 点间隔分离 (EPSS)、前 MV 瓣叶在其最前开口偏移处(E 点)与室间隔之间的距离是一种可重复、快速且高度敏感的测量方法严重的左心室收缩功能障碍。Indeed, both the diastolic excursion of the mitral leaflets and the subsequent degree of closure during systole are intimately related to the vigor of left ventricular systole.
事实上,二尖瓣的舒张期偏移和随后的收缩期闭合程度都与左心室收缩的活力密切相关。重度二尖瓣狭窄时,失去了 E-F,前后叶形成的锯齿样的图消失,变成了长方形样的图,EF Slope 斜率变得非常平缓;后叶的运动不再和前叶相反,而是类似的方向运动;D 和 E 的漂移明显缩短。
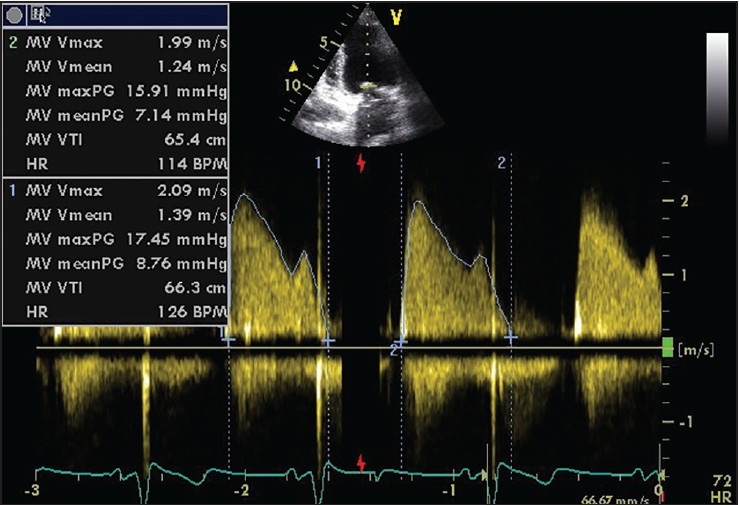
# Mean Pressure Gradient
- The mean pressure difference between the LA and LV
左房左室之间的平均压力差 - Assessed in apical 4 chamber
心尖四腔心测得 - Continuous wave doppler at MV annulus
二尖瓣环处的连续波多普勒 - Trace around MV inflow above the baseline
在基线以上追踪二尖瓣流入端
| Mild | < 5mmHg |
| Moderate | 5-10mmHg |
| Severe | > 10mmHg |
- Affected by: 受以下因素影响:
Decrease in MPG: 偏低
- LA dilatation/ diastolic dysfunction
左房扩张 / 舒张期功能障碍 - Slow heart rate
心率过慢 - Aortic regurgitation
主动脉瓣反流
- LA dilatation/ diastolic dysfunction
Increase in MPG: 偏高
- Rapid Heart rate
心率过快 - Increased transvalvular flow e.g. MR.
跨瓣血流增加,如二尖瓣反流
- Rapid Heart rate
# Mitral Valve Area
# Planimetry 平面测量
- Assessed in PSAX at basal level 在 PSAX 基底水平进行评估
- Trace inner edge of MV orifice in mid-diastole
在舒张中期追踪描绘二尖瓣开口的内缘 - Measure at the leaflet tips.
在瓣叶尖端测量

Limitations: 限制
- May not image true orifice
可能无法成像真实的瓣口 - High gain = overestimate MS
高增益 = 高估 MS - Low gain = underestimate MS
低增益 = 低估 MS - 对操作者经验要求较高,对于有严重钙化的患者不太推荐
- May not image true orifice
优点:
- Best correlations to anatomic MV area
与解剖二尖瓣面积有很好的相关性,有经验的测量者会得到相对精确的测量值 - Less dependant on flow, heart rate and chamber compliance
对血流、心率和心室顺应性的依赖性较小 - Not influenced by concomitant MR
不受合并的 MR 的影响 - Most reliable tool to estimate MS after percutaneous balloon mitral commissurotomy.
评估经皮二尖瓣球囊扩张术后二尖瓣狭窄情况的最可靠工具。
- Best correlations to anatomic MV area
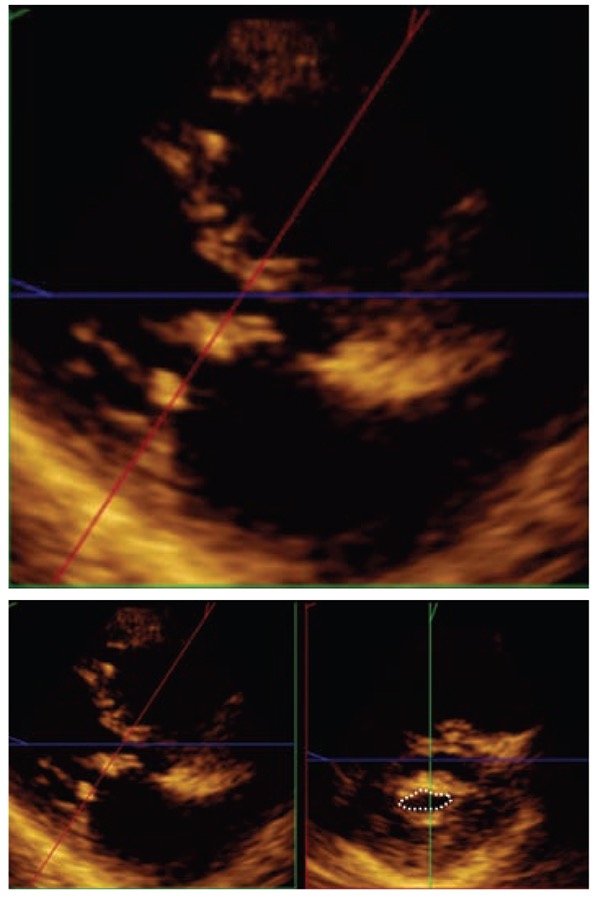
# 3D Echo Planimetry 三维超声优化
Allows optimisation of the position of the sagittal plane in relation to the MV orifice which increases the accuracy
可以对二尖瓣口相对于矢状面位置进行优化,从而提高精度![PLAX(首选)或 4CH,根据平面测量。两个正交视图(红色和绿色)用于验证在二尖瓣小叶上进行了平面测量。]()
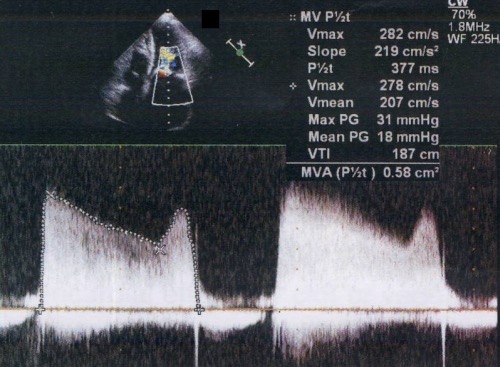
# Pressure Half Time (PHT)
Interval in ms between the maximum mitral gradient and when the gradient is half the initial value.
最大二尖瓣压差与压差为初始值一半之间的时间间隔(毫秒)。Assessed in apical 4 chamber
在心尖四腔进行评估CW at mitral valve annulus
二尖瓣环处的 CWEstimation of MVA using PHT
使用 PHT 估算 MVA
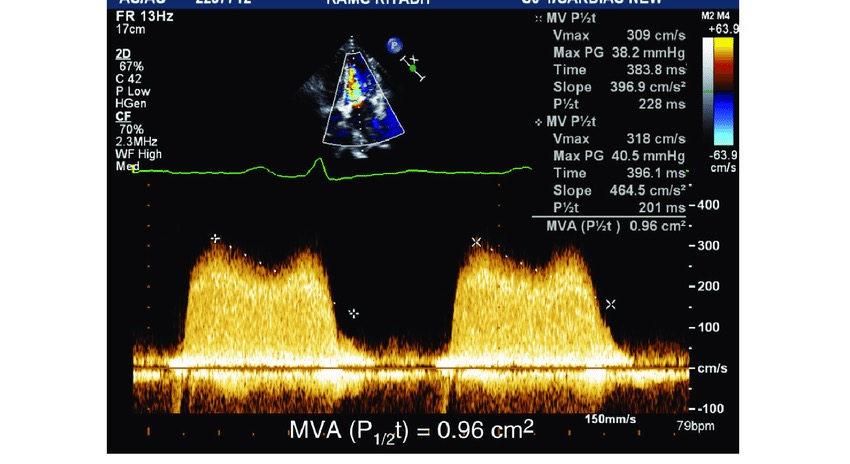
斜率越陡峭,PHT 越短,MVA 越大
斜率平缓,时间延长,PHT 显著增加,MVA 越小
测量时,左侧的起点星型标记放在 E 峰顶点,直线顺着减速的斜坡进行测量,忽略了 A 波的峰值。
PHT 对频谱形态要求较高,当出现凹凸不平或者出现凹陷,会导致测量困难及不精确,这是局限性之一
- Limitations of PHT
Cannot be used post percutaneous balloon mitral commissurotomy
经皮球囊二尖瓣交界分离术后不能使用Rapid LA pressure decline shortens PHT, e.g. ASD, stiff LA
左房压力快速下降会缩短 PHT,例如房间隔缺损、左房僵硬Rapid LV pressure rise shortens PHT, e.g. AR, diastolic dysfunction.
左室压力快速升高会缩短 PHT,例如主动脉瓣反流、舒张功能障碍。All factors that affect pressure half time shorten it.
所有影响压力减半的因素都会缩短它。May lead to overestimation of MVA but PHT can never be underestimated. Therefore, if PHT >220ms, the MS is severe.
可能导致高估 MVA,但 PHT 永远不会被低估。因此,如果 PHT > 220ms,MS 是重度的。
| Normal | 4-6 cm2 |
| Mild MVA | 1.5-2.5 cm2 |
| Moderate MVA | 1.0-1.5 cm2 |
| Severe MVA | < 1.0 cm2 |
如果二维平面测量和多普勒测量值不符合时,尽量多种方法评估瓣口面积,因为每个方法都有局限性,需要综合评判
# Continuity Equation 连续方程
- Can be used if there is discordance between other methods
如果其他方法之间存在不一致,则可以使用 - Estimate functional MV area (instead of anatomic MV area)
估计功能性 MV 面积 (而不是解剖性 MV 面积) - Doppler volumetric method cannot be used in the presence of more than mild AR or MR.
在存在超过轻度 AR 或 MR 的情况下,不能使用多普勒容积法。
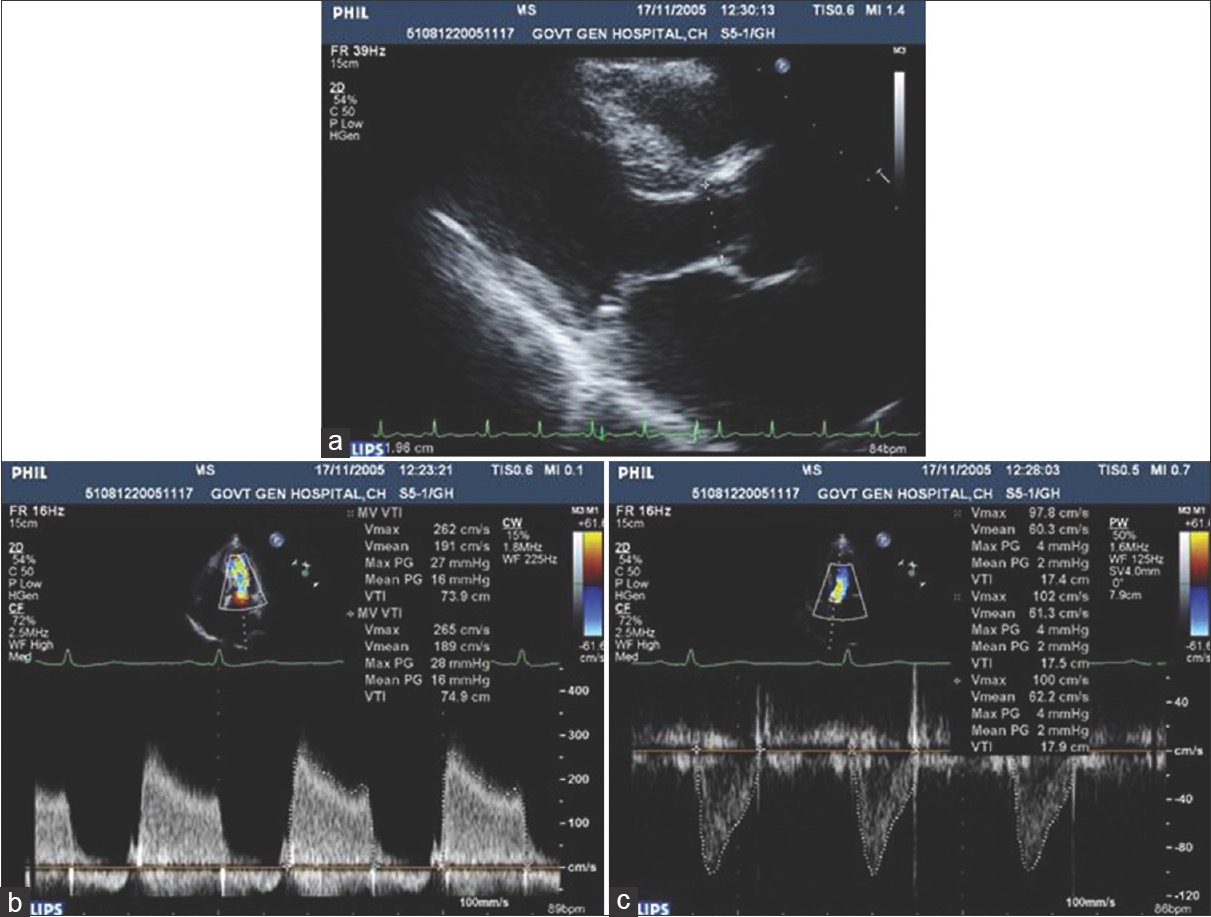
- Mitral valve area by continuity equation [5]
- (a) parasternal long-axis view to measure the left ventricular outflow tract diameter = 1.96 cm
胸骨旁长轴切面测量左心室流出道内径 - (b) A4C view to measure mitral stenosis velocity time integral = 74.9 cm,
A4C 切面测量二尖瓣狭窄速度时间积分 (斜率测量线放置参见前述) - (c) A5C view to measure left ventricular outflow tract velocity time integral = 17.4 cm
A5C 切面测量左室流出道速度时间积分
- (a) parasternal long-axis view to measure the left ventricular outflow tract diameter = 1.96 cm
# Proximal Isovelocity Surface Area (PISA)
- Can be used to calculate MV area
- Zoom in at MV leaflets 在瓣叶水平放大
- Aliasing velocity to 30-40cm/s 上移混叠速度(与 MR 相反)
- Freeze in diastole 在舒张期冻结
- PISA measured at the atrial side 在心房侧测量 PISA
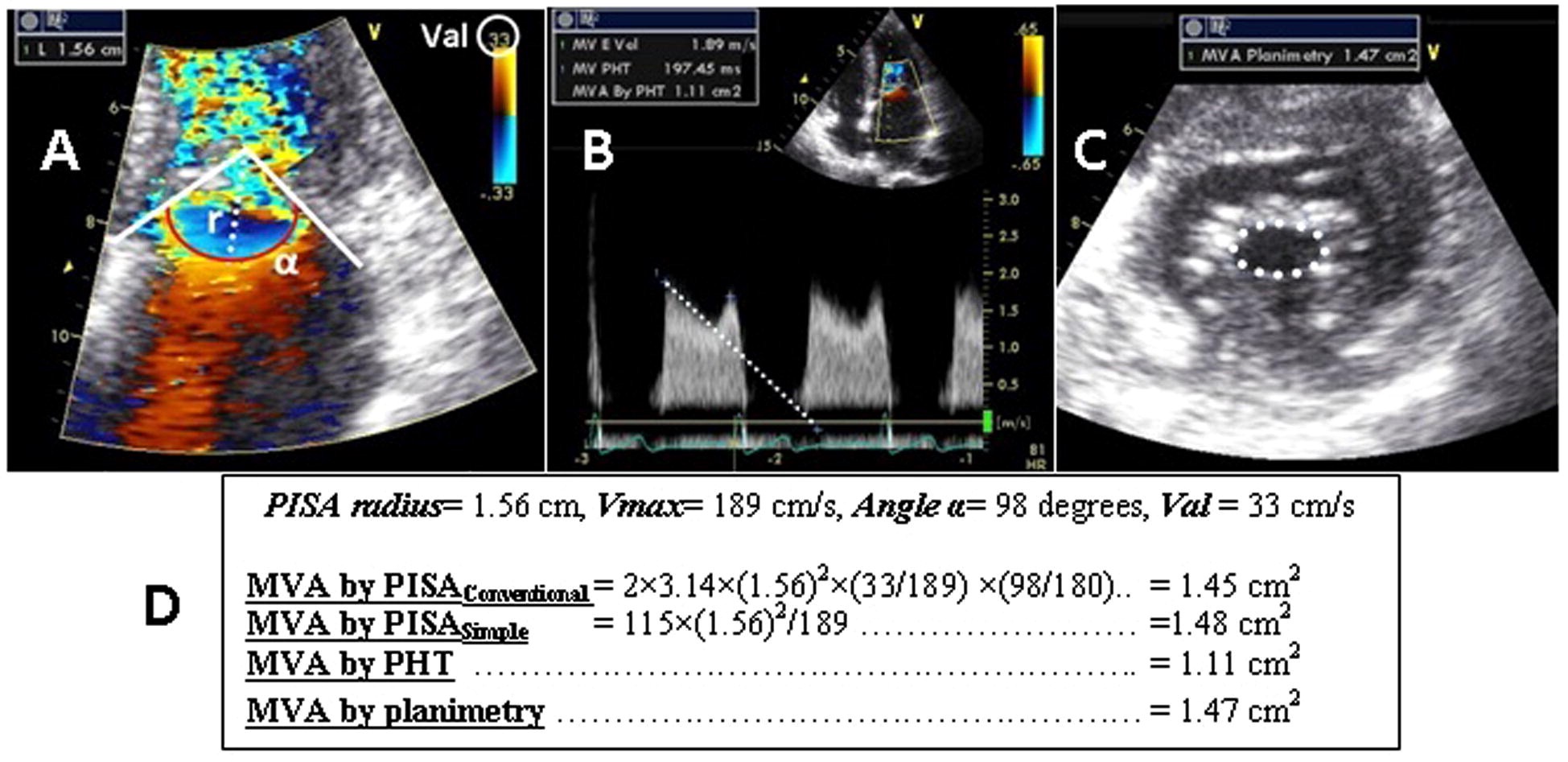
- Calculation of mitral valve area (MVA) by different methods; 用不同方法计算二尖瓣面积(MVA)[6]
- A, proximal isovelcoity surface area method (PISA), 近端等速表面积法(PISA)
- B: pressure half time method (PHT), 压力半时间法(PHT)
- C, the planimetry method (PLN), 平面测量法(PLN)
- D, an example of calculation of MVA by different methods showing good agreement between PLN, PISAconventional and PISAsimple, which was not the case for PHT.
MVA 计算示例通过不同的方法显示 PLN、PISA 常规和 PISA 简单之间的良好一致性,而 PHT 并非如此 - r (cm) is the radius of the PISA cap, Val (cm/s) is the aliasing velocity of color Doppler, Vmax (cm/s) is the maximal velocity across the mitral valve in early diastole (i.e. maximum velocity of the E-wave), and α (degree) is the mitral valve angle.
r (cm) 是 PISA 帽的半径,Val (cm/s) 是彩色多普勒的混叠速度,Vmax (cm/s) 是舒张早期穿过二尖瓣的最大速度(即 E 波),α(度)是二尖瓣角。
# Mitral Leaflet Separation Index 瓣叶分离指数
- Distance between the tips of the mitral leaflets in PLAX
PLAX 二尖瓣前后瓣叶之间的距离 - Semi-quantitative method for MS severity
MS 严重程度的半定量方法 - Not accurate in patients with heavily calcified mitral valve or post valvuloplasty.
在严重钙化的二尖瓣或瓣膜成形术后的患者中不准确
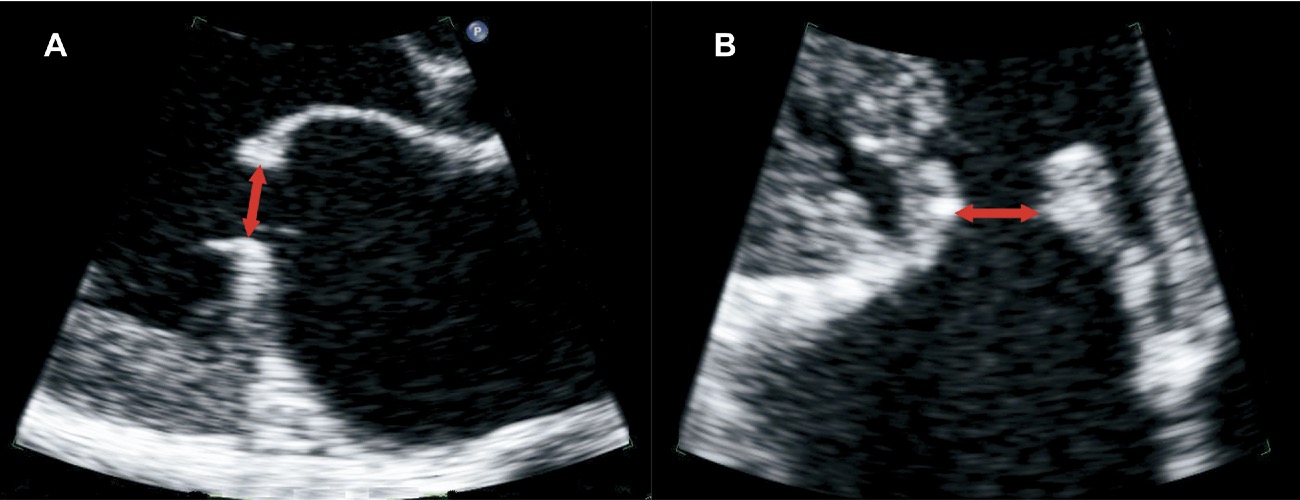
- The MLS index is obtained by averaging the maximal diastolic leaflet separation distance at the tips of the leaflets in parasternal long-axis (A) and (B) four-chamber views. [7]
MLS 指数由胸骨旁长轴切面 (A) 和四腔切面 (B) 瓣叶顶端的最大舒张期瓣叶间隔距离平均得到。
| 1.2cm or more | non-severe MS |
| 0.8cm or less | severe MS |
# 干预指证
# Stress Echocardiography 运动负荷超声心动图
- Exercise testing is indicated in:
- Patients with equivocal symptoms
症状不明确的病人 - Changes in transmitral pressure gradient and PASP during exercise can help select patients for intervention
运动中二尖瓣压差和 PASP 的变化有助于选择患者进行干预 - MPG increase to >15mmHg during exercise = severe MS
运动期间 MPG 增加到 > 15mmHg = 严重 MS - PASP > 60mmHg on exercise is an indication for MVR.
运动时 PASP>60 mmHg 是二尖瓣置换的指征。
- Patients with equivocal symptoms
# Wilkins Score 威尔金斯评分
- Used to assess if percutaneous balloon mitral commissurotomy is suitable [8]
用于评估经皮二尖瓣球囊扩张术是否合适 - Combined score above 8 Suggests the valve may not be amenable to valvuloplasty
综合评分高于 8 分表明该瓣膜可能无法接受瓣膜成形术。
| Apical 4CH | 1 | 4 |
|---|---|---|
| Leaflet mobility | mobile | immobile |
| Leaflet thickening | Normal less than 5mm | Severe thickening >8-10mm |
| Leaflet calcification | No bright echoes | Extensive brightness |
| Subvalvular involvement | Minimal thickening below leaflet tips | Thickening of all chordal structures |
# Commissural Calcification Score 交界区钙化评分
- Useful predictor of outcome in PBMC
PBMC 经皮二尖瓣球囊扩张术结果预测的有用指标- Each half commissure is given a score of 1 if bright echo signal(PSAX Mitral Leaflets)
如果有明亮的回声信号,每个半个交界处的分数为 1 - Total score graded from 0 - 4 (O = no calcification; 4 = severe calcification)
总分从 0 到 4 (0 = 无钙化;4 = 严重钙化) - Commissural calcification score of 0-2 predicts higher valve areas post-PBMC
交界区钙化评分 0-2 预示 PBMC 术后瓣膜面积增加 - Good predictor of severe MR post PBMC.
PBMC 后严重 MR 的良好预测指标
- Each half commissure is given a score of 1 if bright echo signal(PSAX Mitral Leaflets)
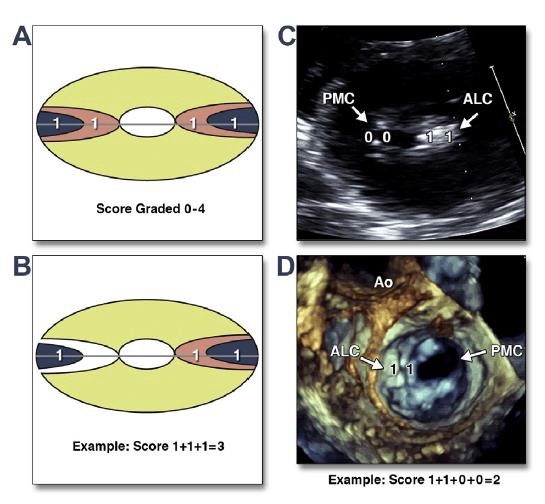
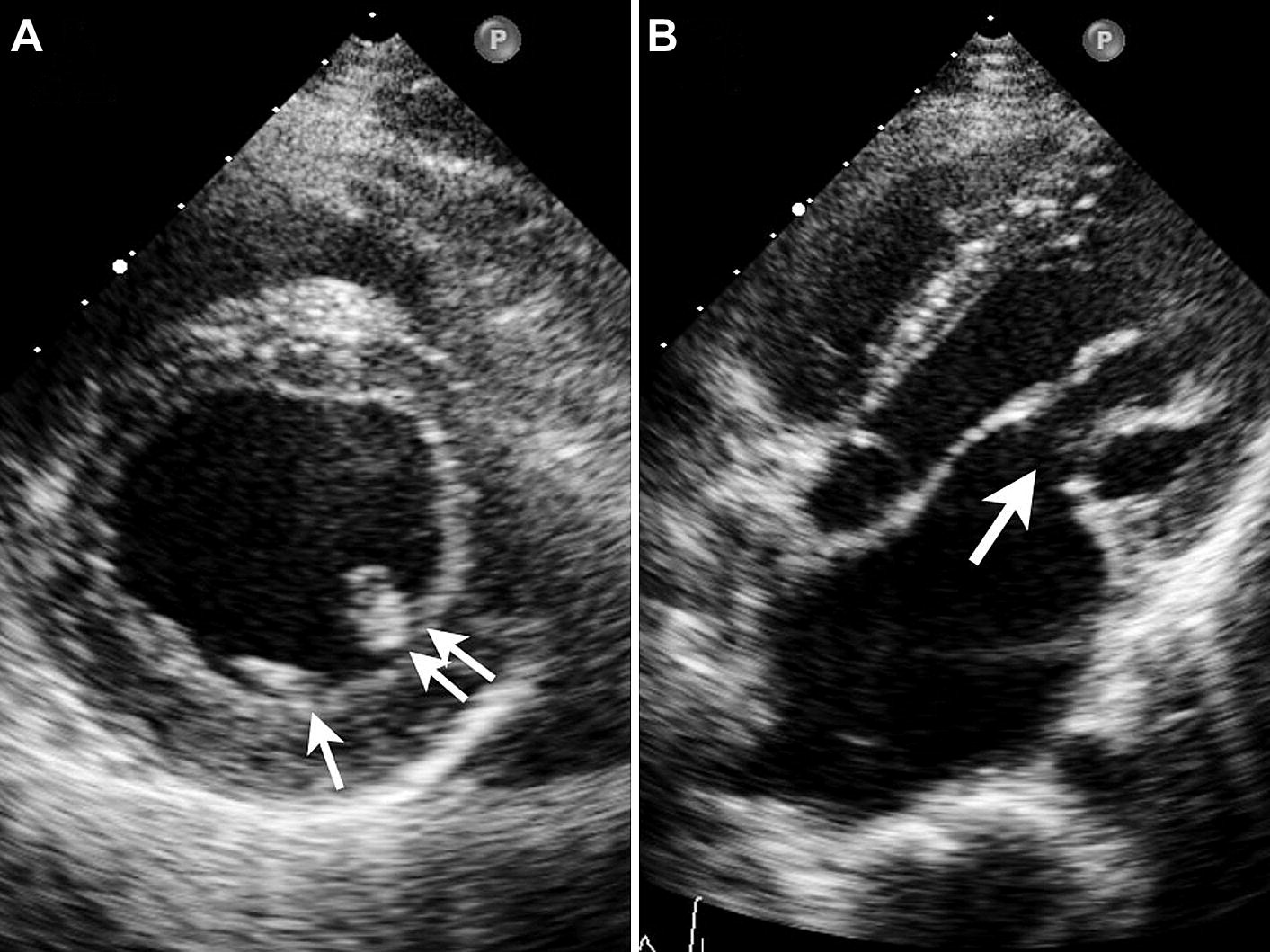
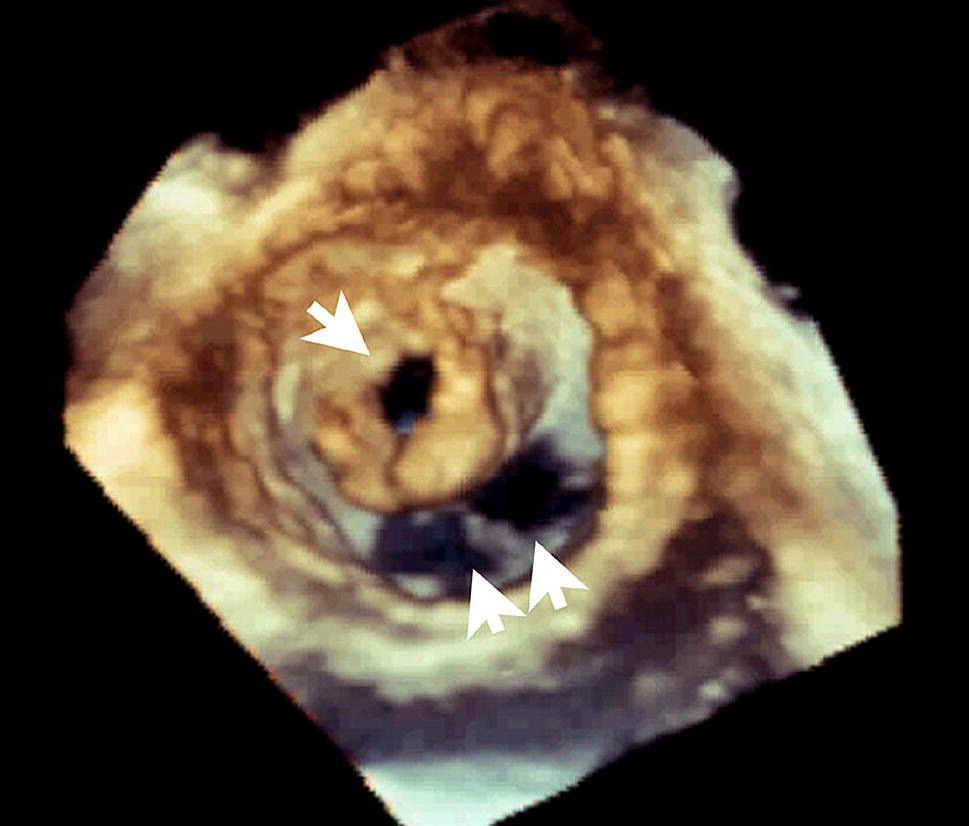
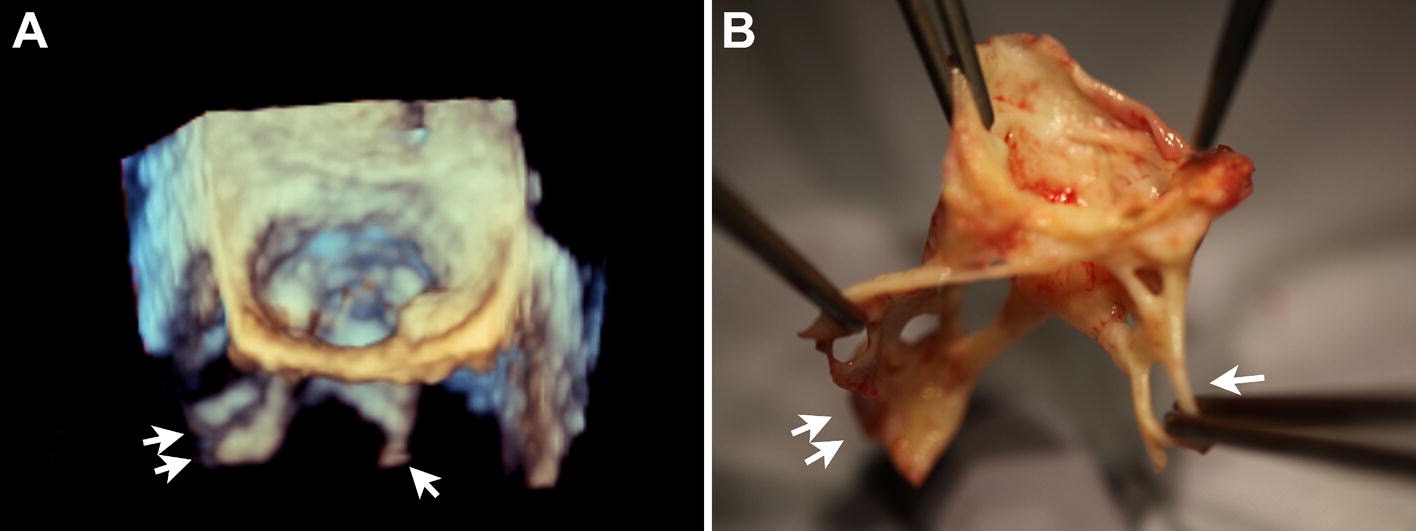
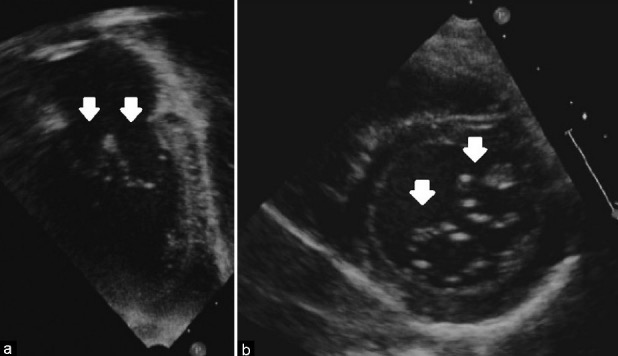
- Commissural calcifications were calculated by assigning each half of the commissures (anterolateral and posteromedial) with detectable high intensity echo brightness with a score of 1. Commissural calcifications ranged from grade 0 (no calcification) to grade 4. [9]
计算交界区钙化的方法是将每半个交界 (前外侧和后内侧) 分区,可检测到高强度的回声亮度则得分为 1。交界区钙化的范围从 0 级 (无钙化) 到 4 级。- (A) Both commissures were completely calcified. 两个交界区完全钙化。
- (B) An example where half the commissure is calcified on the left side and the entire commissure is calcified on the right side, then the value is 3.
例如,左侧交界的一半钙化,右侧整个交界钙化,则该值为 3。 - (C) 2D PSAX display at the level of the mitral leaflet shows that only 1 commissure is completely calcified, whereas the other commissures do not show calcification.
二尖瓣叶水平的 2D PSAX 检查,只有 1 个交界区完全钙化,其他交界区未显示钙化。 - (D) Left atrial aspect 3D TEE view. The score calculated in this example is 2.
左房 3D TEE。本例中计算的分数为 2。 - ALC = anterolateral commissure; Ao = aorta; PMC = posteromedial commissure.
Jassal, D. S. et al. Association of mitral annular calcification and aortic valve morphology: a substudy of the aortic stenosis progression observation measuring effects of rosuvastatin (ASTRONOMER) study. Eur Heart J 29, 1542–1547 (2008). ↩︎
Toufan, M. & Mahmoudi, S. S. Isolated parachute mitral valve in a 29 years old female; a case report. J Cardiovasc Thorac Res 8, 43–45 (2016). ↩︎
Feng, T.-Y. et al. Parachute mitral valve accompanied by bicuspid aortic valve on three-dimensional transesophageal echocardiography. The Kaohsiung Journal of Medical Sciences 28, 506–508 (2012). ↩︎
Remenyi, B. & Gentles, T. L. Congenital mitral valve lesions : Correlation between morphology and imaging. Ann Pediatr Cardiol 5, 3–12 (2012). ↩︎
Ganesan G. How to assess mitral stenosis by echo - A step-by-step approach. J Indian Acad Echocardiogr Cardiovasc Imaging 2017;1:197-205 ↩︎
Salem Omar, A. M., Abdel-Rahman, M. A., Tanaka, H. & Rifaie, O. Simplifying proximal isovelocity surface area as an assessment method of mitral valve area in patients with rheumatic mitral stenosis by fixing aliasing velocity and mitral valve angle. Journal of the Saudi Heart Association 25, 9–17 (2013). ↩︎
Holmin, C. et al. Mitral Leaflet Separation Index: A New Method for the Evaluation of the Severity of Mitral Stenosis? Usefulness Before and After Percutaneous Mitral Commissurotomy. Journal of the American Society of Echocardiography 20, 1119–1124 (2007). ↩︎
Wilkins GT, Weyman AE, Abascal VM, Block PC, Palacios IF. Percutaneous balloon dilatation of the mitral valve: an analysis of echocardiographic variables related to outcome and the mechanism of dilatation. Br Heart J. 1988 Oct;60(4):299-308. ↩︎
Sutaria, N., Northridge, D. B. & Shaw, T. R. Significance of commissural calcification on outcome of mitral balloon valvotomy. Heart 84, 398–402 (2000). ↩︎