# Learning objectives
- To understand the epidemiology, aetiology, pathophysiology and proghosis of aortic stenosis
了解主动脉瓣狭窄的流行病学、病原学、病理生理学和预后 - To review the qualitative and quantitative echocardiographic methods available to assess the severity of aortic stenosis
回顾可用于评估主动脉瓣狭窄严重程度的定性和定量超声心动图方法 - To understand the limitations and pitfalls in these methods
了解这些方法的局限性和缺陷 - To appreciate the role of other imaging modalities to complement standard echocardiography in difficult patient subsets.
了解其他成像方式在困难患者亚群中补充标准超声心动图的作用。
# Aortic Stenosis
Most important and common primary valve disease
最重要和最常见的原发性瓣膜病Valvular: 最常见
- Congenital/ Bicuspid valve 先天性 / 二叶式
- Rheumatic 风湿性
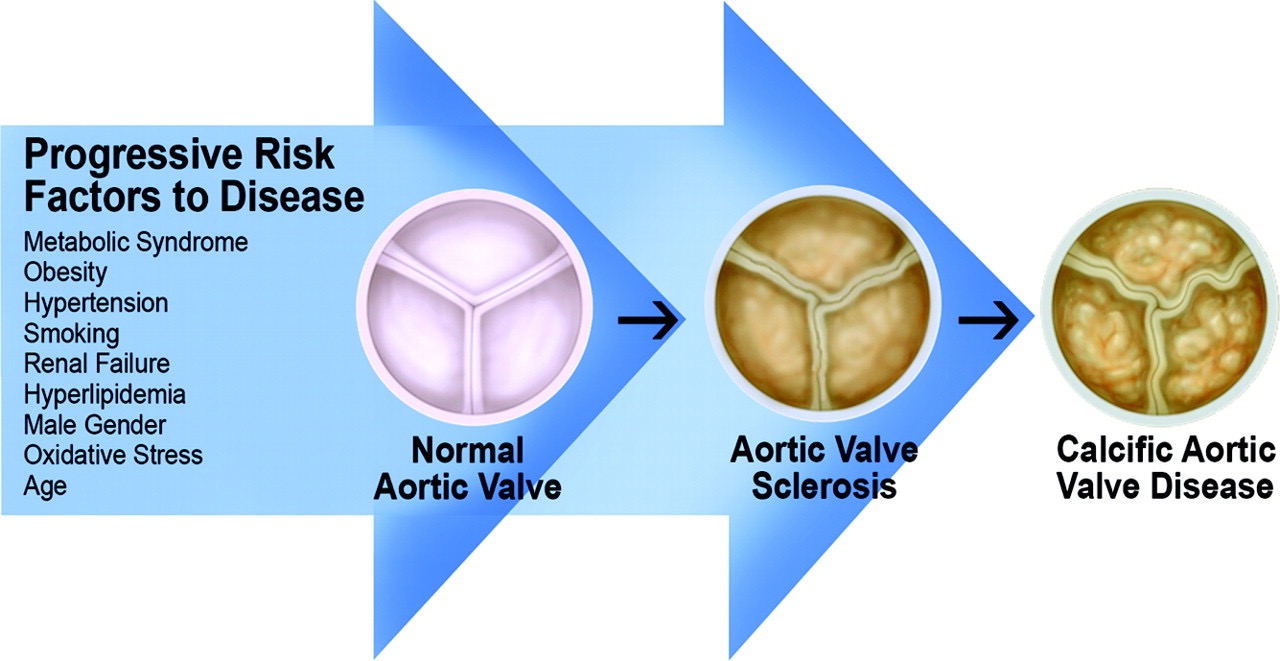
- Calcific degenerative 钙化退行性变
Sub-valvular: 瓣下
- Sub valvular membrane/dynamic muscular obstruction
瓣膜下 / 动力性肌肉阻塞
- Sub valvular membrane/dynamic muscular obstruction
Supra-valvular (uncommon, e.g. Williams Syndrome).
瓣上(罕见,例如威廉姆斯综合征)
# Aortic Valve Pathology
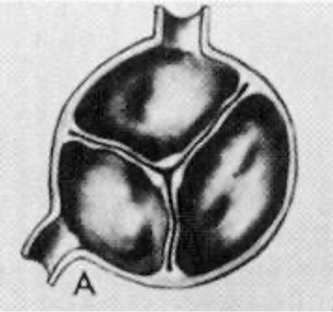


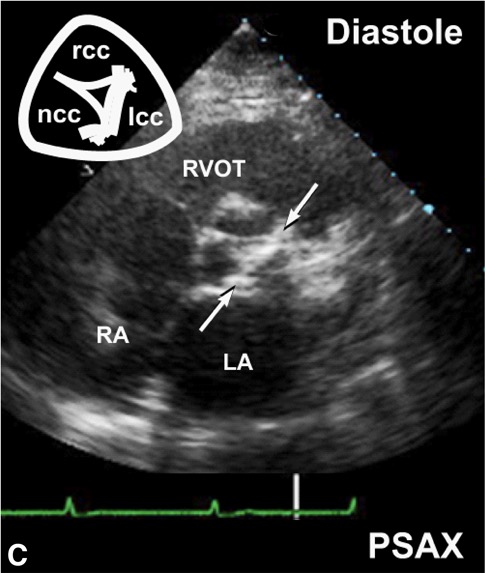
# Bicuspid Valve
- Most often (80%) fusion of the left and right coronary cusps; large anterior cusp
最常见的是(80%)左右冠瓣融合成,大的前瓣 - Fusion of the right and non-coronary cusps less common (20%); large right cusp
右冠瓣和无冠瓣融合较少 (20%);表现为较大的右冠瓣 - Fusion of left and non-coronary cusps (2 equal sized cusps) is rare; “true bicuspid valve"
左冠瓣和无冠瓣融合 (2 个大小相等的瓣叶) 是罕见的;表现为 “真正的二尖瓣” - Best to see in systole with fused and closed cusp; diastolic images confused by presence of a raphe.
最好在收缩期观察瓣叶融合和关闭(SAX 典型的鱼嘴样);舒张期图像可因脊缝的存在而出现混淆。 [1]
![Sketch showing bicuspid aortic valve variants with different commissural orientations (parasternal short-axis views [PSAX]).显示具有不同连合方向的二叶主动脉瓣变体的草图(胸骨旁短轴视图)。](https://s2.loli.net/2022/09/24/ugCsbDpAxeFRQOJ.jpg)
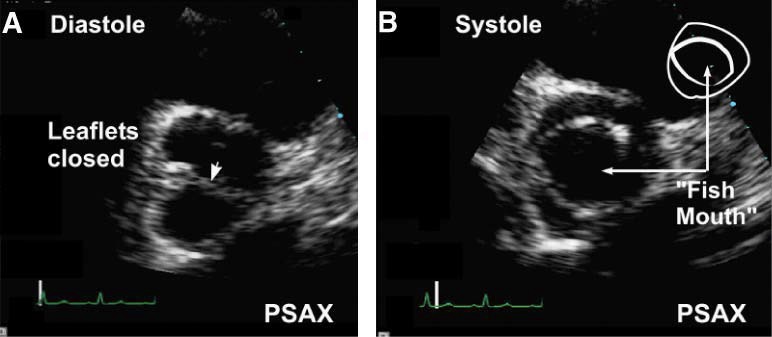
![Bicuspid aortic valve during diastole (A) and systole (B) in parasternal short-axis (PSAX) view. Note horizontal commissure (arrow) in diastole and “fish mouth” appearance during systole. (C,D) Systolic doming of bicuspid aortic valve during systole (parasternal long-axis view [PLAX]). 在胸骨旁短轴 (PSAX) 视图中,舒张期 (A) 和收缩期 (B) 的二叶式主动脉瓣。注意舒张期的水平连合 (箭头) 和收缩期的 “鱼嘴” 外观。(C,D) 收缩期二叶式主动脉瓣穹隆样改变 (胸骨旁长轴视图)。](https://s2.loli.net/2022/09/24/ZPElveQY46xI5r9.jpg)
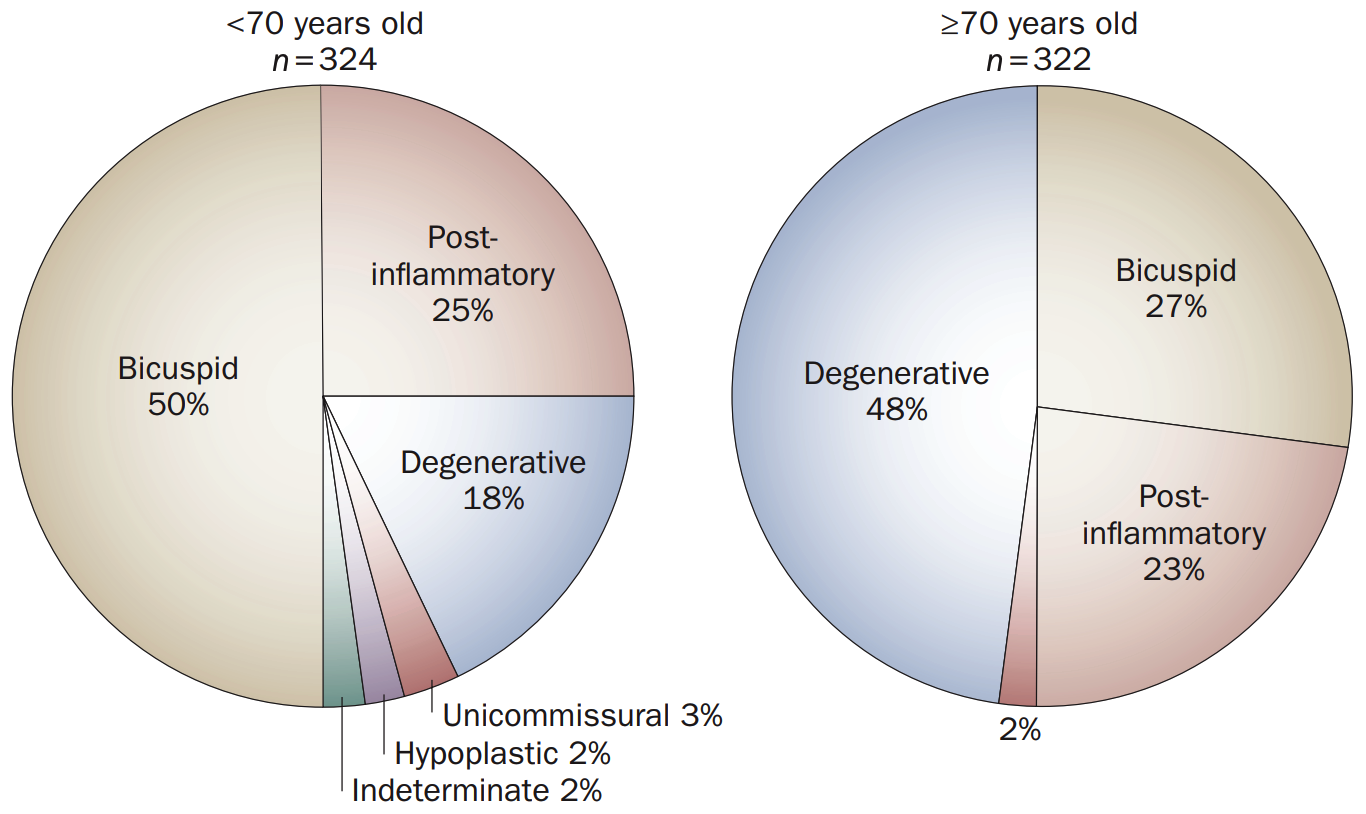
# Aortic Stenosis Demographics 人口统计学
Aortic stenosis: 主动脉瓣狭窄
- 2% US population > 65 years old
Aortic sclerosis: 主动脉瓣硬化
- 29% US population > 65 years old
- 50% greater risk of mortality and myocardial infarction.
死亡和心肌梗死的风险增加 50%。
Aortic sclerosis progresses to aortic stenosis in 9% over 5 years. [2]
主动脉瓣硬化在 5 年内进展为主动脉瓣狭窄的比例为 9%。
# Echocardiography/Doppler
- Valve morphology 瓣膜形态
- LV dimensions - function 左室内径以及功能
- Haemodynamic measurements 血流动力学评估
- Associated lesions 相关病变

# Two-Dimensional Assessment
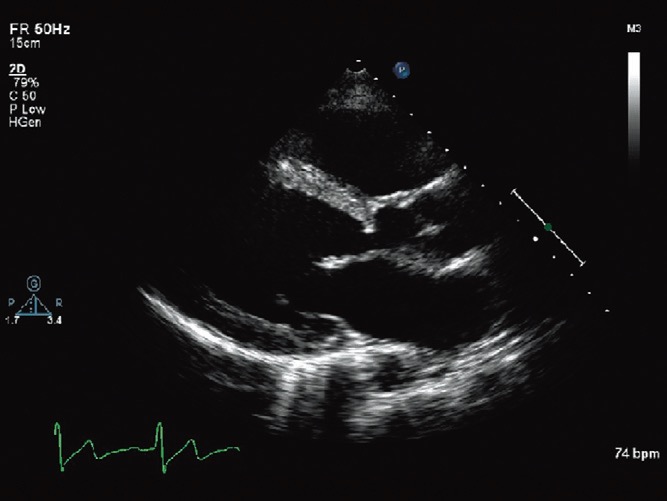
# 2D echo PLAX
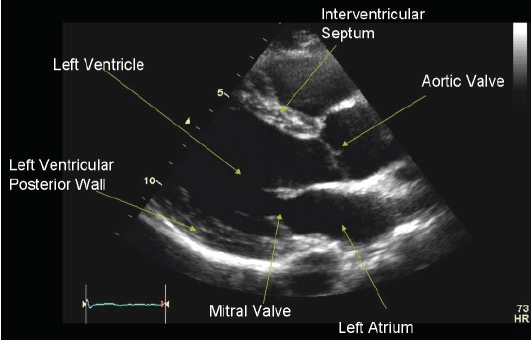
NCC(above) and LCC(bottom)
上方为无冠瓣,下方为左冠瓣,看不到右冠瓣Doming/asymmetric closure line (bicuspid)?
穹隆样改变 / 不对称闭合线(二叶式)?Fusion of commissures (? Rheumatic)
交界融合(风湿性)?Leaflet thickening/ severity (mild/moderate/severe)
瓣叶增厚 / 严重程度 (轻度 / 中度 / 重度)
Mobility: Leaflet restriction
移动度:瓣叶限制- Mild - Restricted as basal third
限制局限在根部的三分之一 - Moderate - base and body
瓣叶根部和瓣叶体 - Severe - Entire leaflet
整个瓣叶
- Mild - Restricted as basal third
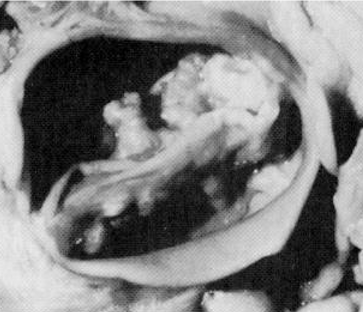
Leaflet calcification
瓣叶钙化- Severity 严重程度
- Mild - Small isolated spots 孤立的小钙化点
- Moderate - Multiple larger spots 多个较大的钙化点
- Severe - Extensive calcification 广泛钙化
- Location and extent 位置和范围
- AV cusps - free edge, body or point of insertion
主瓣瓣尖 - 无边缘、瓣体或插入点 - LVOT - annulus, aortic wall, aortic root, ascending aorta.
LVOT - 瓣环,主动脉壁,主动脉根,升主动脉。
- AV cusps - free edge, body or point of insertion
- Severity 严重程度
2D Measurements 测量指标
- LVOT - Zoom, mid systole, inner edge to inner edge
左室流出道 - 放大,收缩中期,内缘到内缘 - Annulus 瓣环
- The measurement is VITAL for the calculatior for calculation of aortic valve area
该测量对于计算主动脉瓣面积是至关重要的 - As the measurement is squared it is the greatest source of error.
测量值会被平方,是最大的误差来源
- LVOT - Zoom, mid systole, inner edge to inner edge
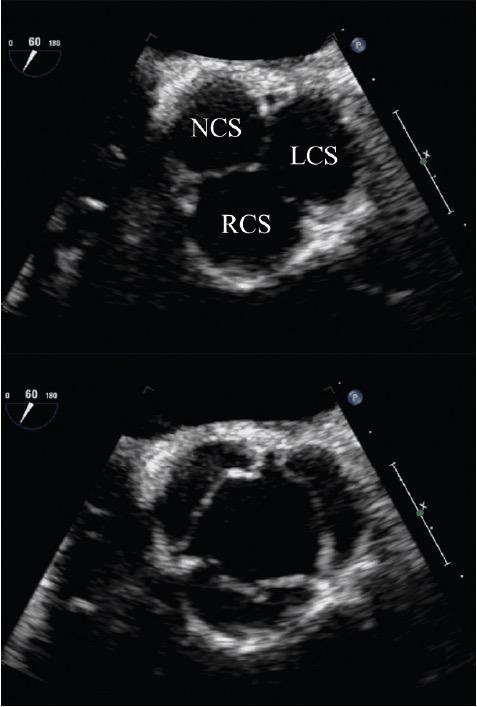
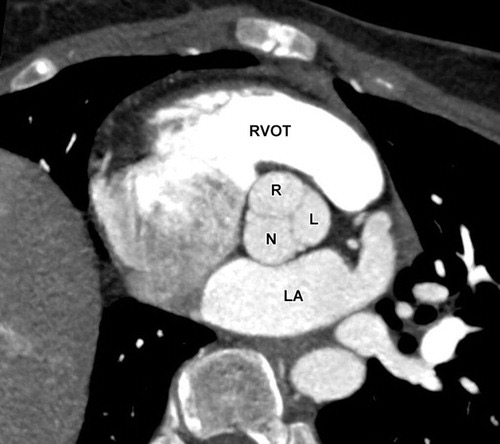
# 2D echo PSAX
- NCC, LCC and RCC
- Assess number of cusps in congenital abnormality
评估先天畸形的瓣尖数目 (leaflet variations) - Calcification mobility as on PLAX.
同 PLAX 上的钙化活动度观察




# Colour Flow Mapping 彩色多普勒
Can be used in PLAX or Apical views
Ensure turbulent flow as expected at valve level - if below? LVOT obstruction
确保瓣膜水平的湍流符合预期 -- 如果低于?则考虑左心室流出道梗阻Ensure turbulent flow is at valve level rather than above or below the valve itself.
确保湍流处于瓣膜水平,而不是高于或低于瓣膜本身。Sub-aortic membrane [3]
瓣下膜性结构导致了狭窄

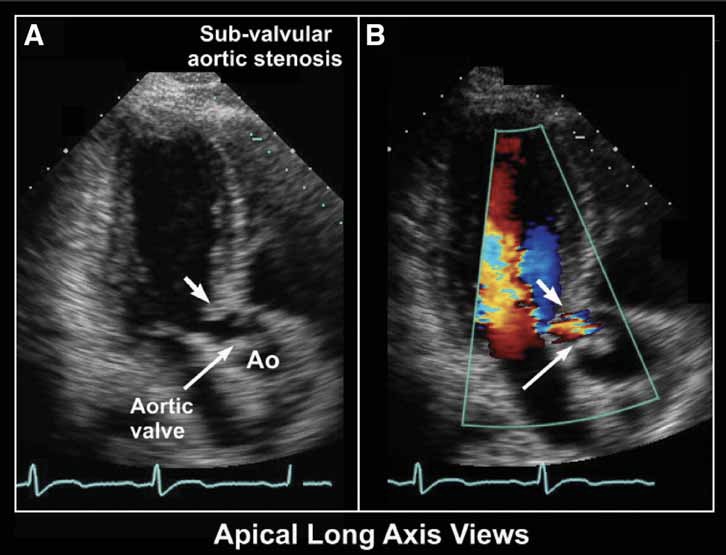
- LVOT 梗阻的 CW 表现
# Annulus Dimensions
- Increasingly important for valve sizing for TAVI
TAVI 瓣膜尺寸的选择日益重要 - 2D or 3D TOE better than TTE
经食道优于经胸 - CT generally widest-used technique to also yield information about coronary anatomy, shape of the aortic root, distance between coronaries and the valve, and information about the peripheral vasculature.
CT 通常是最广泛使用的技术,还可以提供有关冠状动脉解剖、主动脉根部形状、冠脉和瓣膜之间的距离以及周围血管的信息。
# Aortic Valve Planimetry 主动脉瓣平面测量
- Inaccurate as depends on cut level
不准确,因为取决于切面水平 - Try to find level with MINIMAL area
尝试找到面积最小的水平 - “'Effective" rather than "anatomical' area is primary predictor with outcome
“有效” 面积而不是 “解剖” 面积是预后的主要预测因素 - Suggest not to pursue as a primary measure
建议不要将其作为主要措施 - May be considered with 3D or TOE examination.
可考虑进行 3D 或经食道检查。
# The Bernoulli Equation
- Principle of conservation of energy
能量守恒原理
V1 = proximal velocity 近端速度
V2 = distal velocity 近端速度
= density of fluid (g/cm3)
dv = velocity change over time
ds = distance over which pressure decreases
R = viscous resistance in vessel(g/cm4/sec)
- if V1 < 1.5m/s can simplify
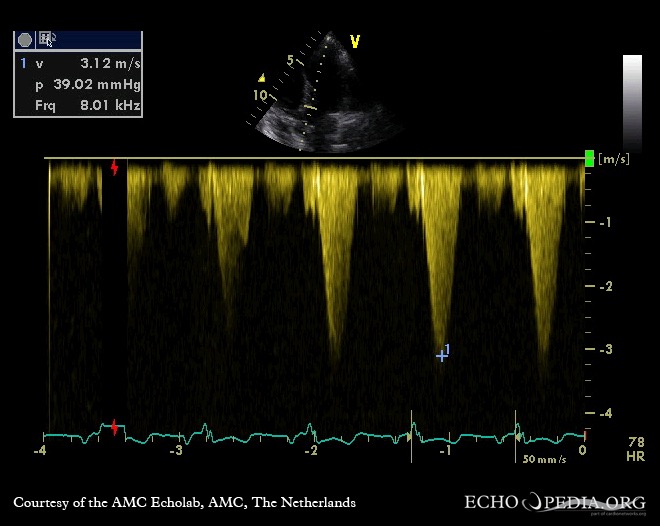
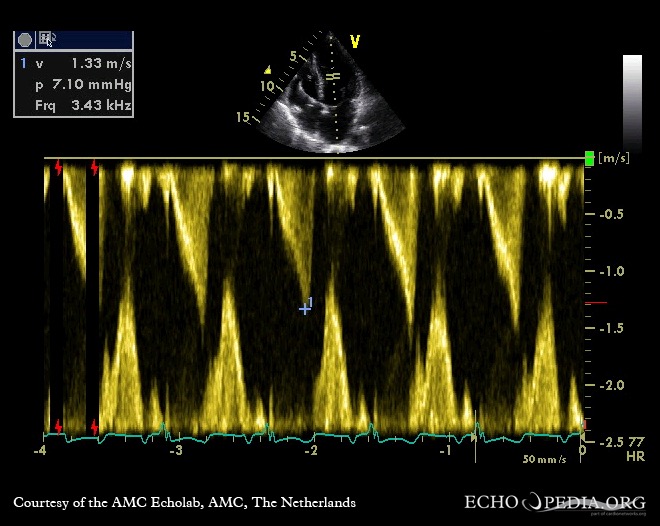
# LVOT
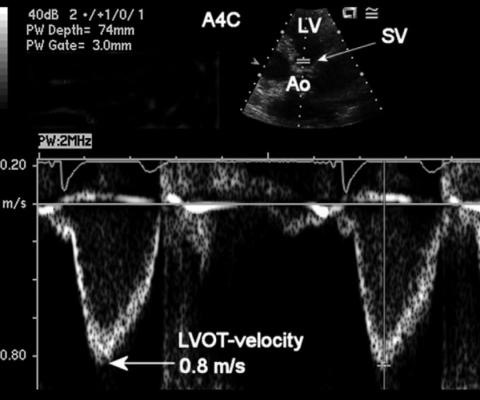
- 5C view 五腔心
- 5-10mm on LV side of valve
瓣下心室面 5-10mm - Ensure thin and even velocity profile
确保速度剖面薄而均匀 - Defined peak - measure peak
定义峰值 - 测量峰值 - Measure "mean" for VTI, i.e. mid profile.
测量 VTI 的 “平均值”,即中层轮廓
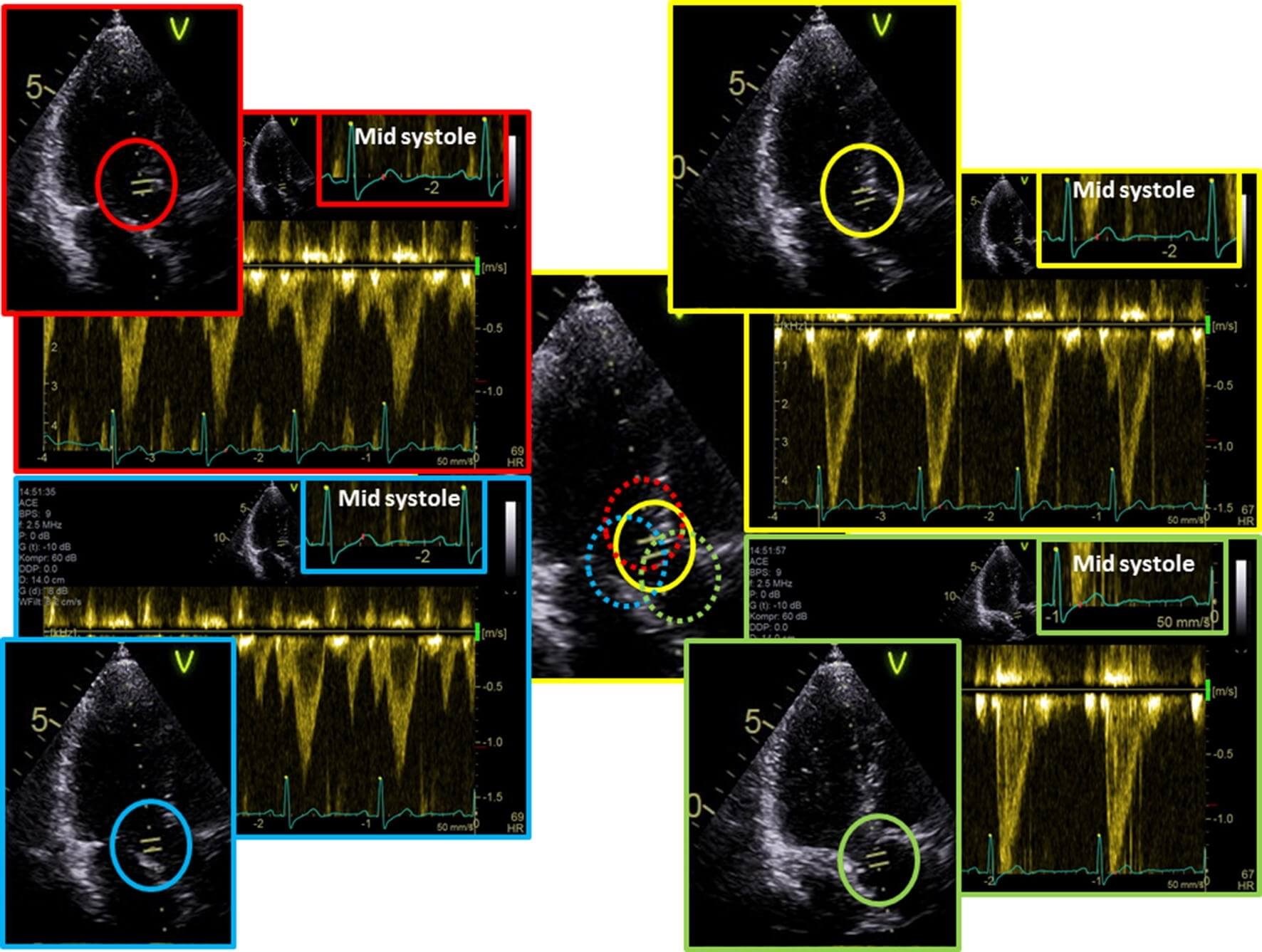
# Peak AV velocity
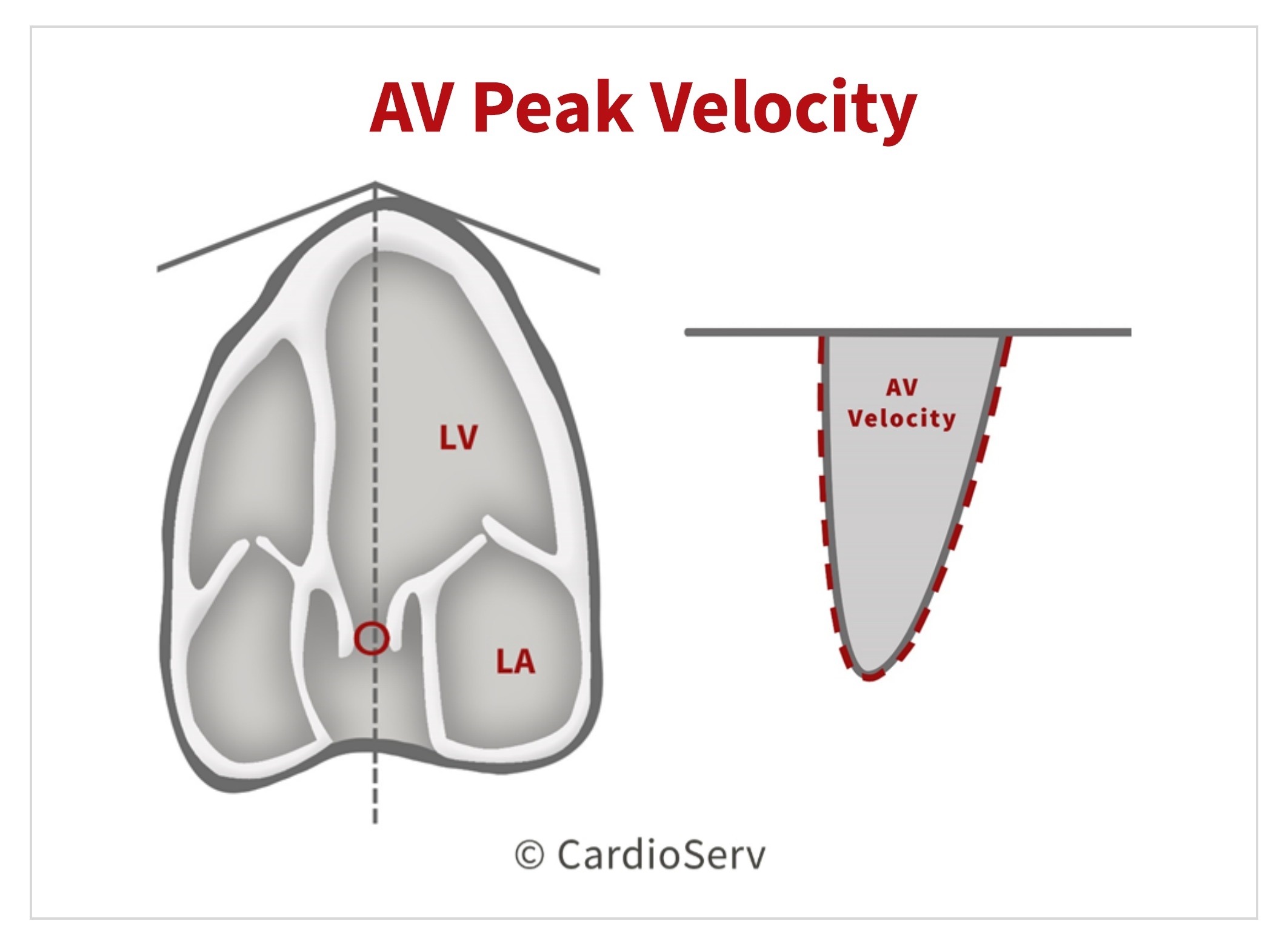
- Multiple views to find highest value
多个切面以查找最大值 - Optimal alignment 最优对齐
- Ignore the fine linear signals
忽略细微的线性信号 - Measure interface.
测量界面
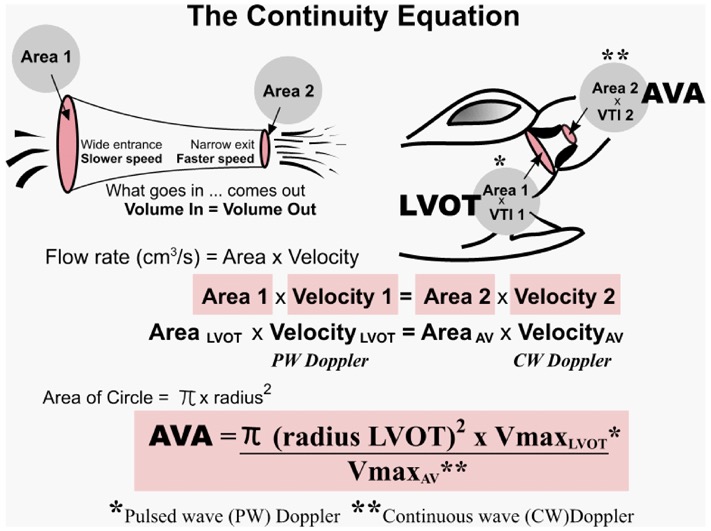
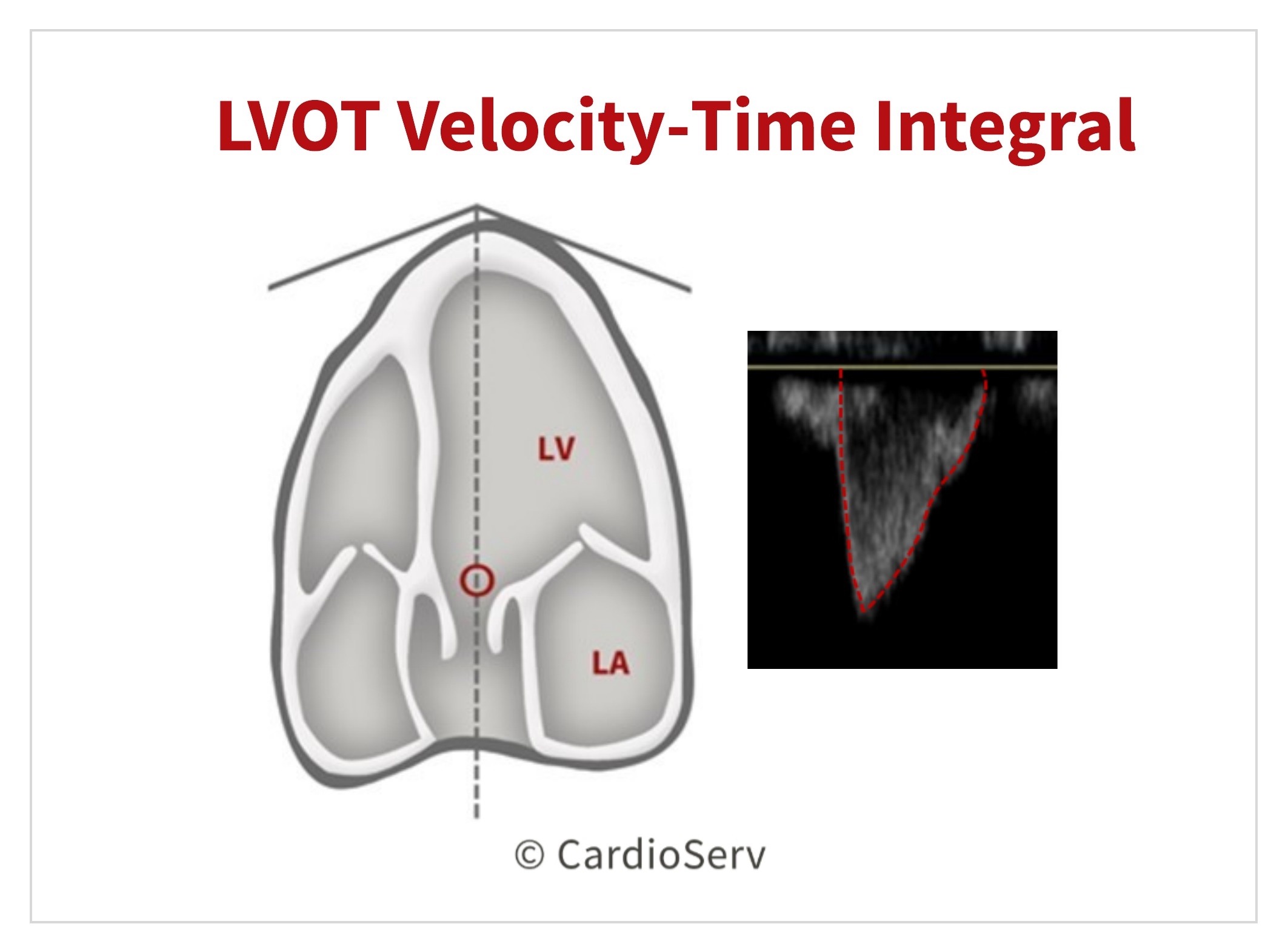
# Haemodynamic measurements 血流动力学评估
- Peak gradient 最大跨瓣压差
Mean gradients derived from and .
平均跨瓣压差来自 和 。Aortic valve area from continuity equation
主动脉瓣面积来自连续方程- Generally do not index AVA unless very small adult
一般来说,除非是体型非常小的成年人,否则不会计算 AVA
![The continuity equation and assumptions for measuring aortic valve area (AVA) in aortic stenosis.主动脉瓣狭窄时测量主动脉瓣面积(AVA)的连续性方程和假设。]()
- Generally do not index AVA unless very small adult
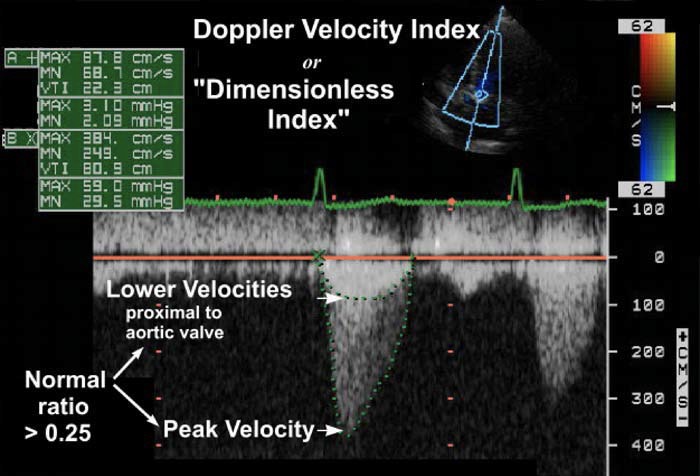
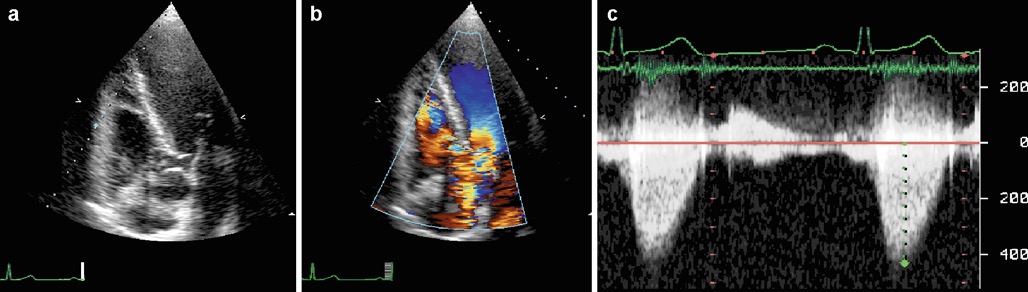
Dimensionless Index Used if LVOT diameter cannot be measured
如果无法测量 LVOT 直径,则使用速度指数![The Doppler velocity index or dimensionless index by CW Doppler across aortic valve. 经主动脉瓣连续波多普勒测定血流速度指数或无量纲指数。]()
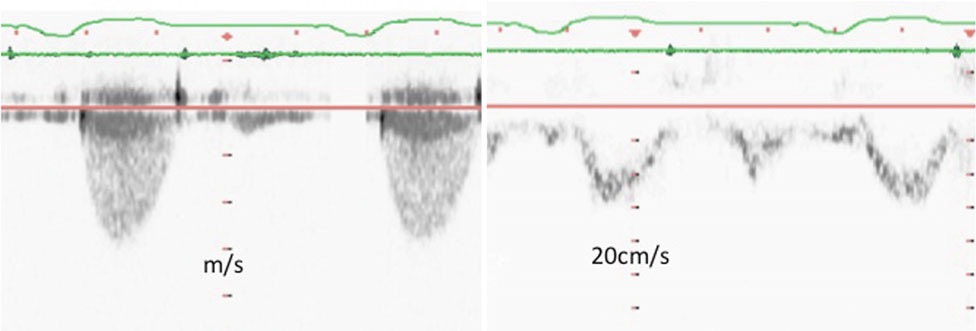
- The continuous-wave Doppler envelope shows a peak velocity of 3.8 m/s across aortic valve.
连续波多普勒显示主动脉瓣的峰值速度为 3.8 m/s。 - The velocity proximal to the valve (depicted by the bright lower velocities highlighted by the arrow) reached 87 cm/s.
瓣膜近端的速度 (用箭头标出的明亮的较低速度表示) 达到 87cm/s. - The ratio of the latter to the former is less than 0.25.
后者与前者的比率不到 0.25。 - This Doppler velocity index, also known as dimensionless index, is normally more than 0.25, but decreases with significant valve stenosis.
该多普勒速度指数 (也称为无量纲指数) 通常大于 0.25,但随着明显的瓣膜狭窄而降低。
- The continuous-wave Doppler envelope shows a peak velocity of 3.8 m/s across aortic valve.
# Tips and Tricks
# Outflow Tract Measurements 流出道径线测量
Inner edge to inner edge
Strictly LVOT measure 0.5-1 cm from AV orifice
In practice this may be inaccurate as LVOT is non-circular and dynamic
在实践中,这可能是不准确的,因为 LVOT 是非圆的和动态的Correlations with CT AVA made
Ideally in mid-systole 收缩中期
Annulus MUST BE PERPENDICULAR and ON AXIS
切瓣环的切面必须垂直且同轴IGNORE CALCIFICATION In the measurement
测量中忽略钙化
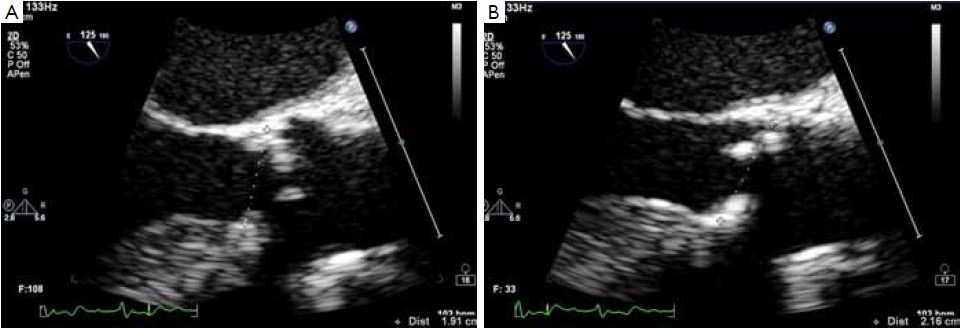
- A. The annulus is measured as the distance between the hinge point of the cusps and calcifications are included in the measurement. In this picture, the correct section of the left ventricle outflow tract and of the aortic root is shown; [4]
瓣环测量的是瓣叶铰链点之间的距离,钙化包括在测量中。A 图显示了左心室流出道和主动脉根部的正确测量切面; - B. A common mistake. The aortic valve cusps are not symmetrically cut. In this case the hinge point of the non-coronary cusp (upper one) is not at the nadir of the cusp, but on the ascending part of the insertion line in the aortic root. This error leads to a significant overestimation of the annulus (in this particular patient, 19 mm in A vs. 22 mm in B)
一个常见的错误。主动脉瓣瓣叶没有对称切开。在这种情况下,无冠瓣的铰链点 (上端) 不在瓣叶的最低点,而是在主动脉根部插入线的上升部分。这一错误导致了对瓣环径的严重高估 (在这个特殊的患者中,A 环为 19 mm,B 环为 22 mm)
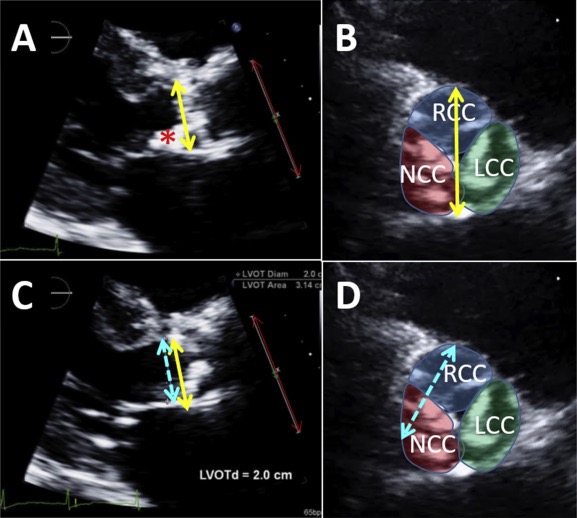
The original figure legend suggests that measurement in panel A would result in an incorrectly small annulus, but the largest diameter of the annulus is obtained from panel A (yellow double arrow) by excluding the ectopic calcium (red asterisk) extending onto the anterior mitral valve leaflet. [5]
原图 A 中的测量会导致不正确的偏小瓣环,但最大的瓣环直径是通过排除延伸到二尖瓣前叶的异位钙化(红色星号)从图 A(黄色双箭头)获得的。Panel B is a representation of where that measurement would be taken from the short-axis view.
B 图表示将从短轴切面中获取该测量值的位置。The same yellow arrow from panel A superimposed onto panel C is longer than the suggested measurement (dashed blue arrow).
叠加到图 C 上的图 A 的相同黄色箭头,比建议的测量 (蓝色虚线箭头) 更长。Panel D is a representation of where that incorrect measurement would be taken from the short-axis view, with the two calcified cusps centered in the aortic root.
图 D 显示了从短轴视图进行不正确测量的位置,两个钙化的瓣叶于主动脉根部的中心。LCC, Left coronary cusp; LVOTd, LVOT diameter; NCC, noncoronary cusp; RCC, right coronary cusp.
Underestimation of LVOTO diameter: AVA will be falsely low
低估 LVOTO 直径:主瓣面积也会被错误的低估Underestimation of the stroke volume will lead to a diagnosis of Low Flow Low Gradient AS
低估每搏输出量将导致诊断为低流量低压差的主动脉瓣狭窄Consider: 考虑
- Recheck LVOT measurement 重新检查 LVOT 的测量
- TOE and look at valve morphology 经食道和观察瓣膜的形态
- Use alternative techniques - CT. 使用替代技术
# Aortic valve area 主动脉瓣面积
Recent update of the European Association of Cardiovascular Imaging and American Society of Echocardiography recommendations
Should we measure LVOT diameter at annulus or 0.5-1 cm below in annulus at same level as PW measurement?
我们应该在瓣环水平测量 LVOT 直径,还是在与 PW 测量位置相同的瓣环水平下 0.5-1cm 测?Historically, LVOT measurement made at the annulus and there is strong outcomes data using this method
从历史上看,LVOT 测量是在瓣环水平进行的,使用这种方法有很强的结果数据支持MSCT studies have now confirmed that the aortic valve annulus as well as LVOT are elliptical in most patients
CT 已证实,大多数患者的主动脉瓣环以及 LVOT 是椭圆形的Annulus less dynamic and less elliptical in systole
瓣环在收缩期更少动态,更小椭圆Recent data suggest that more precise measurement of AVA using MSCT LVOT area may be of particular importance in low gradient AS to avoid misclassification of AS severity patients
最近的数据表明,在低压差 AS 中,使用 MSCT 测 LVOT 面积能更精确,能避免严重患者的误分类Use 3D echocardiography: Directly planimetry but note decreased spatial resolution with 3DE.
使用 3D 超声心动图:直接平面测量,但注意到 3D 超声降低了空间分辨率。
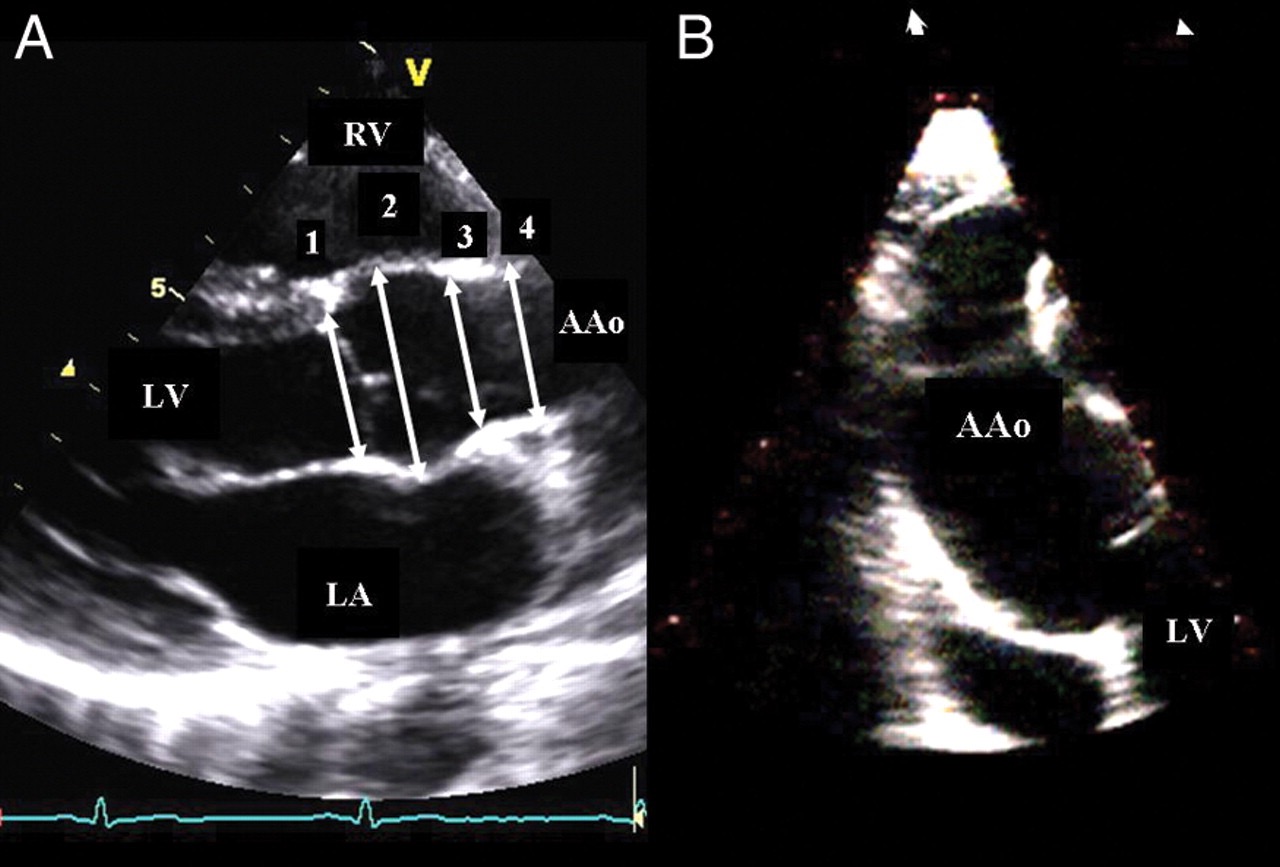
- (A) Parasternal long-axis view (transthoracic echocardiography). The following diameters are shown: outflow tract diameter (1), sinuses of Valsalva (2), sinotubular junction (3), and tubular ascending aorta (4). [5:1]
胸骨旁长轴切面 (经胸超声心动图)。流出道直径 (1)(这是老的,现在 LVOT 在 (1) 所示瓣环下 0.5-1cm 测)、Valsalva 窦 (2)、窦状交界处 (3) 和管状升主动脉 (4)。 - (B) Right parasternal long-axis view, mid and distal parts of ascending aorta may be visualized.
右侧胸骨旁长轴切面,可见升主动脉的中部和远端。 - AAo, ascending aorta; LA, left atrium; LV, left ventricle; RV, right ventricle.
# LVOT velocity
Underestimation 低估
- Non-parallel alignment 未平行对齐(CW 和 PW 与角度有很大依赖性,要在彩色多普勒的指引下,尽量放置在线性关系比较好的部位)
- Sample volume too far from LVOT 取样容积离 LVOT 太远
Overestimation 高估
- Sample volume too close to valve with proximal flow convergence
取样容积太接近近端流动收敛的瓣膜 (越靠近越被高估) - Sub-aortic obstruction e.g. dynamic obstruction with basal septal hypertrophy
主动脉瓣下梗阻,例如伴有基底室间隔肥厚的动态梗阻
- Sample volume too close to valve with proximal flow convergence
High LVOT velocity e.g. AR or high Cardiac Output
高左室流出道速度,例如存在主动脉瓣反流或高心排血量- Cannot use Simplified Bernoulli equation as V1 cannot be ignored
不能使用简化的伯努利方程,因为不能忽略 V1 - Can use . 可以使用改良版的
- Cannot use Simplified Bernoulli equation as V1 cannot be ignored
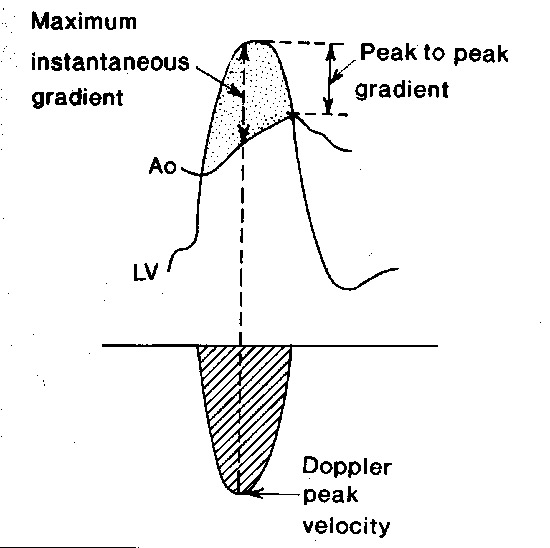
- Difference in catheterisation and echo gradients.
心导管和超声测得压差的区别,因为心导管测的是最大跨瓣压差(peak to peak),心超测的是瞬时压差(peak instantaneous)
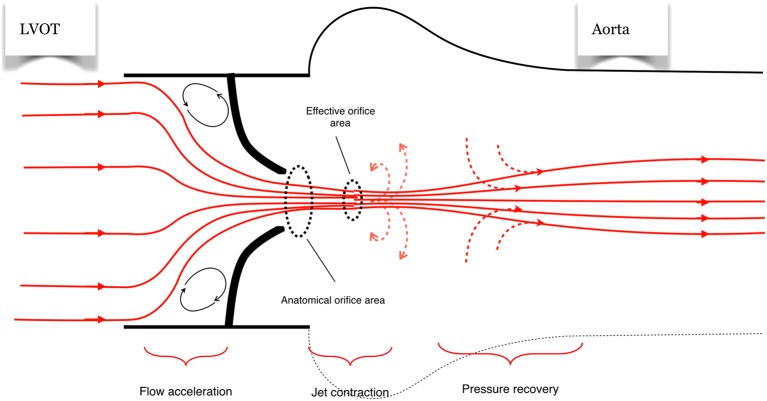
- Note that continuity equation is measurement of effective orifice area not anatomical area - differences due to flow effects through narrow orifice.
注意,连续性方程计算的是有效瓣口面积的测量值,而不是解剖面积 - 由于通过狭窄瓣口的流动效应而产生的差异 - Good clinical outcome correlation with this ERO rather than anatomical area.
良好的临床结果与 ERO 相关,而不是与解剖区域相关。
# AS velocity
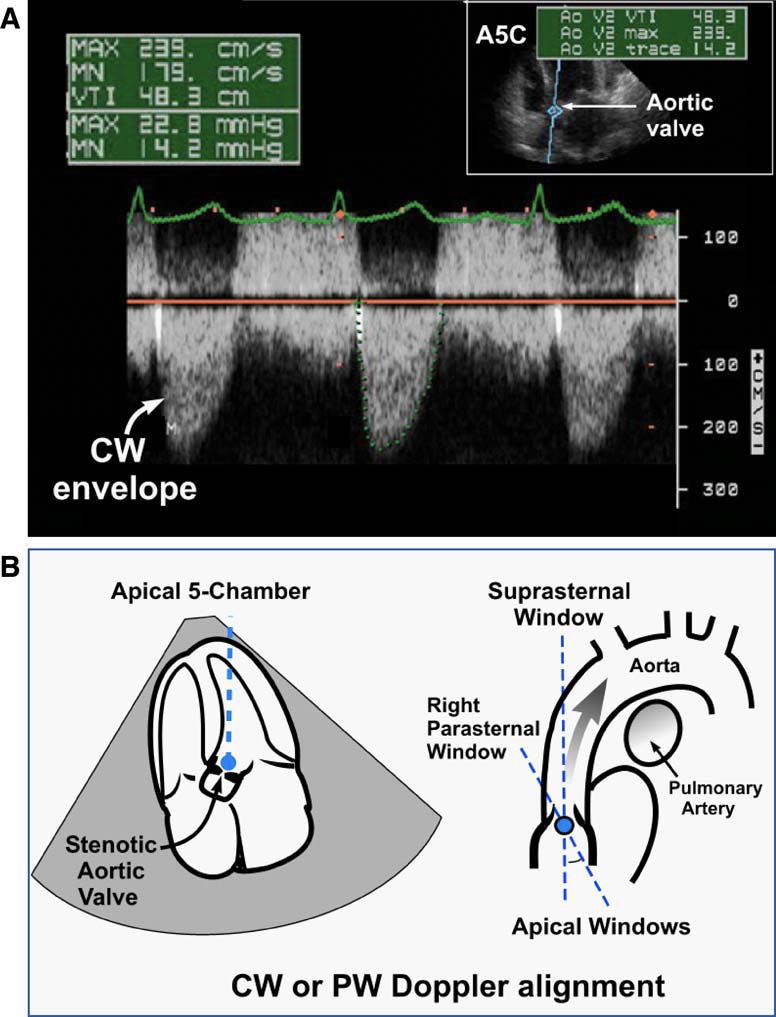
Use multiple acoustic windows: Apical 5c, Suprasternal and Right Parasternal - choose highest velocity window (alignment)
使用多个声窗:心尖五腔心、胸骨上和胸骨右旁 - 选择最高速度窗口 (对齐)Adjust scale, baseline, gain and filter
调整比例、基线、增益和滤波Use colour flow imaging to identify the optimal positioning of the cursor
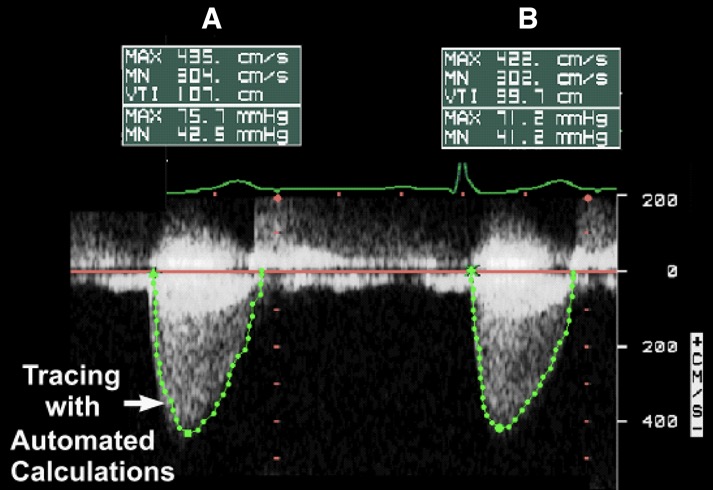
使用彩色血流成像来确定光标的最佳位置CW Doppler
Parallel intercept with jet 与反流束平行
Measure max and VTI 测量最大值和 VTI
Use dense part not fine linear signals the peak (transit-time effect)
使用密集的部分,而不是细微的线性信号峰值
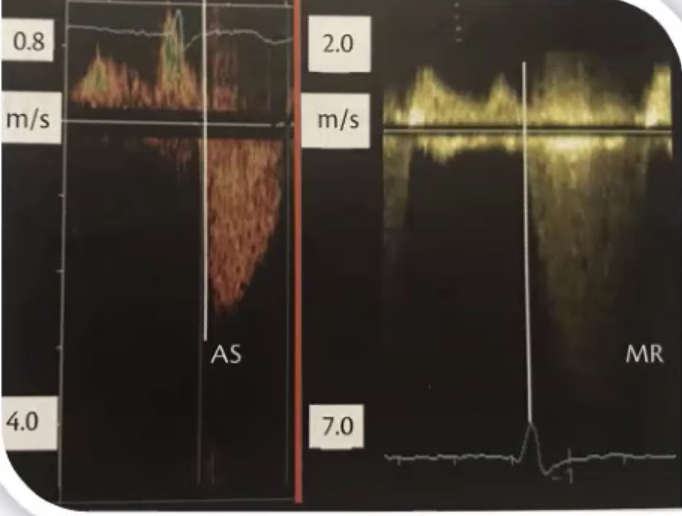
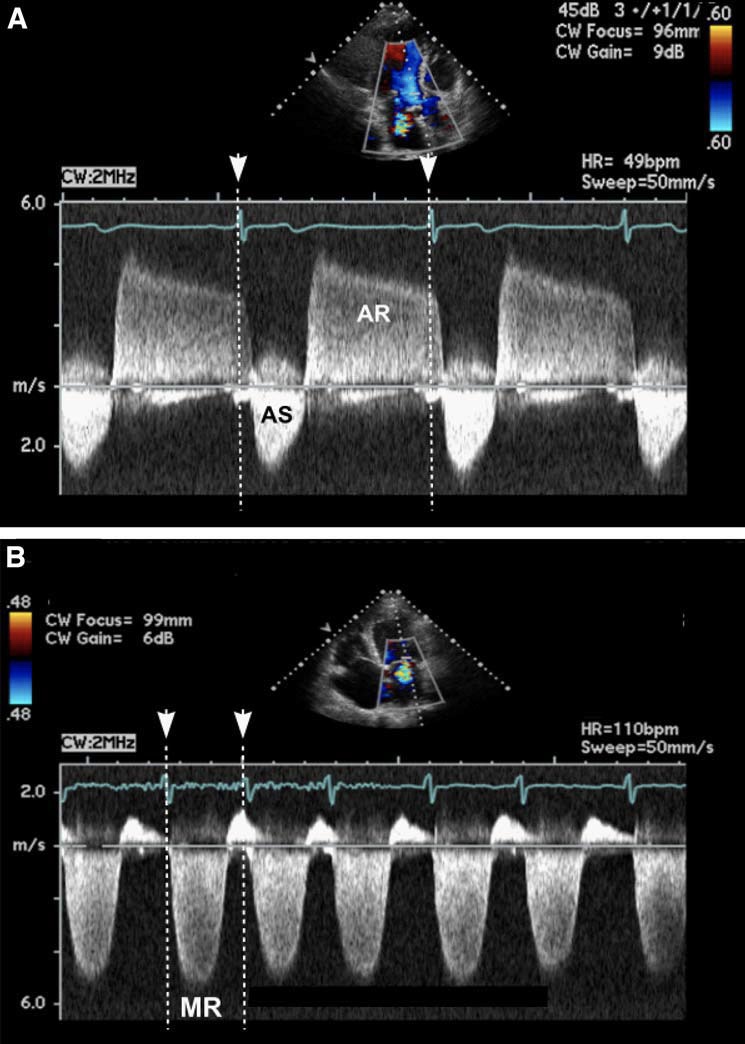
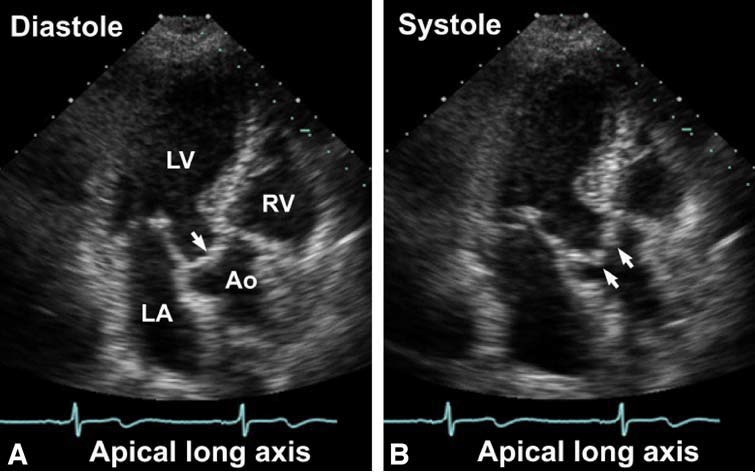
- Do NOT confuse with MR: 不要与二尖瓣反流混淆:
- Both jets both occur in systole and appear as downward spectral velocity shifts when recorded from the apex. [1:1]
两种射流都发生在收缩期,当从心尖记录时,表现为向下的频谱速度偏移。 - The onset of ventricular systole and mitral regurgitation occurs prior to aortic valve opening.In addition, mitral regurgitation is longer in duration.
心室收缩和二尖瓣反流发生在主动脉瓣打开之前。此外,二尖瓣返流的持续时间更长。- MR starts earlier 二尖瓣反流开始得更早
- AS only after QRS 主动脉瓣狭窄仅在 QRS 之后
- Both jets both occur in systole and appear as downward spectral velocity shifts when recorded from the apex. [1:1]
# Grades of Severity 严重程度分级
| Sclerosis | Mild AS | Moderate AS | Severe AS | ||
|---|---|---|---|---|---|
| Peak aortic velocity | m/s | < 2.5 | 2.5 - 3 | 3 - 4 | > 4 |
| Mean Gradient | mmHg | Normal | < 25 | 25 - 40 | 40 (US); 50(Europe) |
| Aortic valve area | cm2/m2 | Normal | > 1.5 | 1 - 1.5 | < 1 |
| Dimensionless index | 0.25 | ||||
2014 ACC/AHA guidelines, severe aortic stenosis is defined as ANY OF:
- Aortic valve area (AVA) less than 1.0 cm2
- Mean gradient greater than 40 mmHg
- jet velocity greater than 4.0 m/s
Onset of symptoms 出现症状的瓣口面积
- 0.9 cm2 with CAD
- 0.7 cm2 without CAD
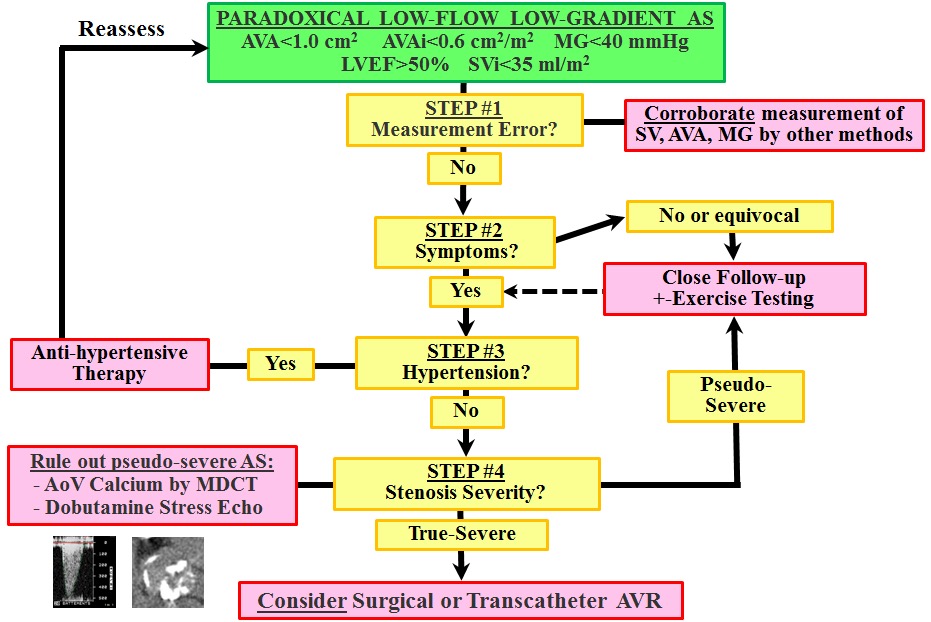
Note that discordances can occur between these 3 criteria for severe AS:
请注意,出现以下情况时,严重主动脉瓣狭窄的三个标准可能互不相符:
Consider- Low ejection fraction 低射血分数
- Difficulties with LVOTO size 左室流出道梗阻
- Low stroke volume states despite preserved LVEF
尽管保留了左心室射血分数,但每搏量较低
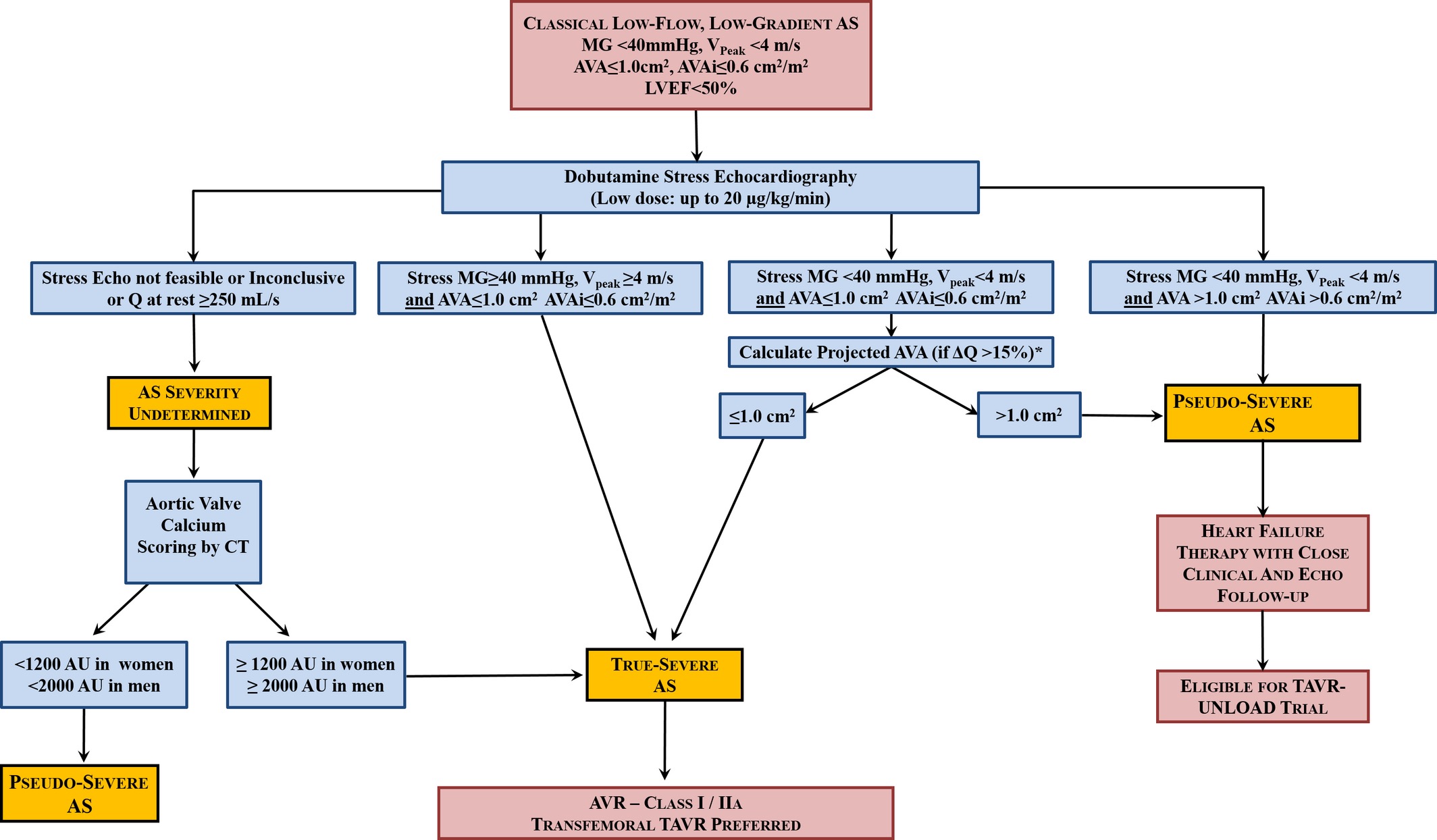
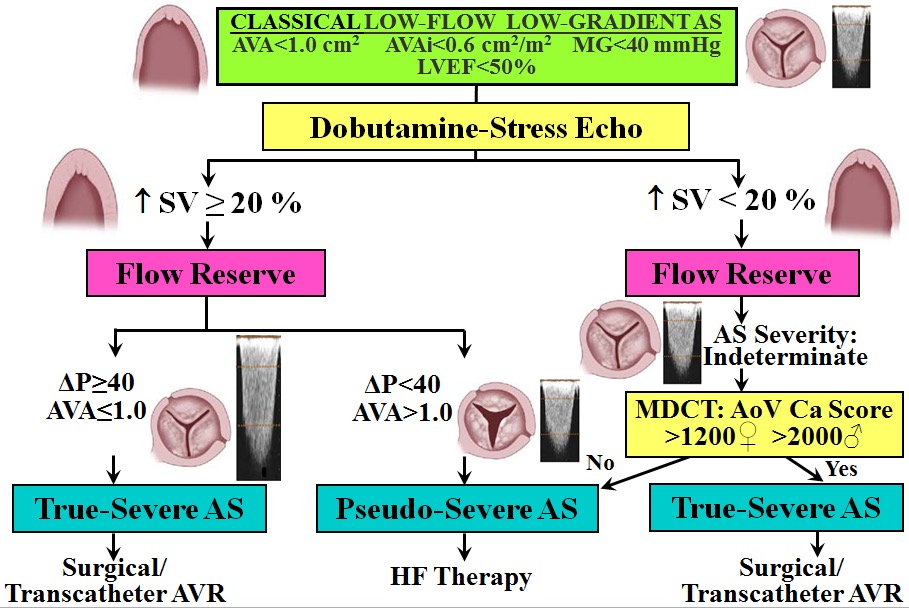
# Classical Low Flow, Low Gradient AS 经典的低血流、低压差主瓣狭窄
Low gradient with a small calculated valve area in the setting of poor systolic function. This may result in lack of referral for AVR because of the low gradient.
在收缩功能较差的情况下,计算的瓣膜面积较小,压差较低。因为压差较低可能会导致忽略主动脉瓣置换的转诊。5 - 10% of the AS population
Definition: 定义
- AVA < 1 cm2
瓣口面积 小于 1 - WITH LVEF < 40% Or stroke volume index < 35ml/m2
左室射血分数降低 或 每搏量指数降低 - AND Transthoracic MPG < 40mmHg.
经胸超声见平均跨瓣压差低
- AVA < 1 cm2
# Aortic Stenosis and Impaired LV Function 主动脉瓣狭窄与左室功能受损
- Is LV dlysfunction the cause or the result of AS?
LV 功能丧失是 AS 的原因还是结果? - Is there separate myocardial dysfunction?
是否有单独的心肌功能障碍? - Is AVR going to improve survival?
AVR 能提高生存率吗?- True severe AS due to afterload mismatch
真正严重的 AS 是由于后负荷不匹配- Valve replacement beneficial most cases
瓣膜置换在大多数情况下是有益的
- Valve replacement beneficial most cases
- Pseudo-severe AS - moderate AS with intrinsic myocardial dysfunction, approximately 33% of these patients
其中约 33% 的患者为假性中重度 AS,合并固有心肌功能障碍- Valve replacement may not be needed.
可能不需要换瓣治疗
- Valve replacement may not be needed.
- True severe AS due to afterload mismatch
# Dobutamine or exercise Stress Echo 多巴酚丁胺负荷超声心动图
- By increasing cardiac output, we can determine if the AS is severe by reassessing the gradient across the aortic valve (increases) AND the aortic valve area (decreases).
通过增加心输出量,可以通过重新评估主动脉瓣的压差 (增加) 和主动脉瓣面积 (减少) 来确定 AS 是否严重。 - Assess myocardial contractile reserve
评估心肌收缩储备- Does the cardiac output improve by 20% or more.
心输出量是否提高 20% 或更多。
- Does the cardiac output improve by 20% or more.
- Critical for decision-making regarding aortic valve replacement.
对主动脉瓣置换术的决策至关重要。
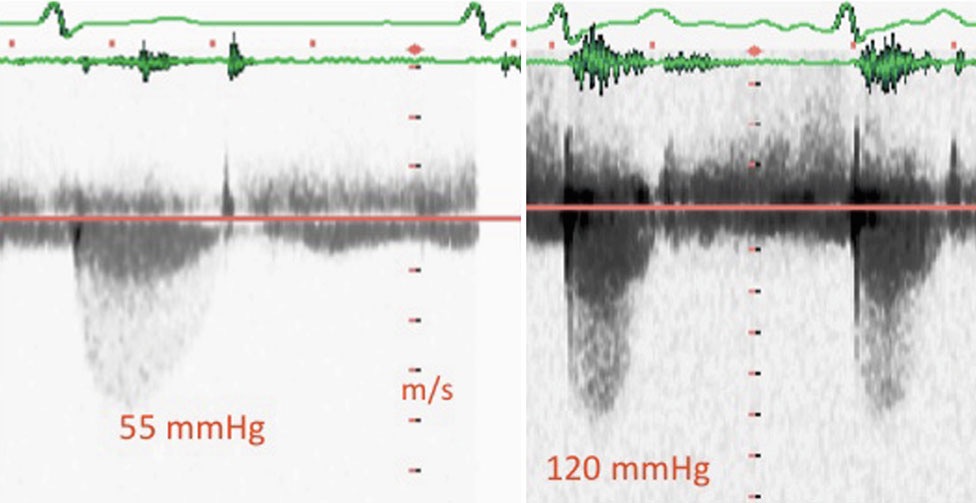
# Management of Classical (low LVEF) LF-LG AS
参考链接
Bermudez, E. A. Echocardiographic Assessment of Aortic Stenosis. in Essential Echocardiography: A Practical Handbook With DVD (eds. Solomon, S. D. & Bulwer, B.) 209–221 (Humana Press, 2007). ↩︎ ↩︎
Rajamannan, N. M. et al. Calcific Aortic Valve Disease: Not Simply a Degenerative Process. Circulation 124, 1783–1791 (2011). ↩︎
Henein, M. Y., Sheppard, M., Pepper, J. R. & Rigby, M. Aortic Valve. in Clinical Echocardiography (ed. Henein, M. Y.) 33–62 (Springer, 2012). ↩︎
Cerillo, A., Mariani, M., Berti, S. & Glauber, M. Sizing the aortic annulus. Annals of Cardiothoracic Surgery 1, 24556–24256 (2012). ↩︎
Hahn, R. T. & Pibarot, P. Accurate Measurement of Left Ventricular Outflow Tract Diameter: Comment on the Updated Recommendations for the Echocardiographic Assessment of Aortic Valve Stenosis. Journal of the American Society of Echocardiography 30, 1038–1041 (2017). ↩︎ ↩︎